Electrocardiography (ECG/EKG) is the graphic recording of the electrical activity (electric potentials) of the heart. It is a noninvasive and affordable method of monitoring, often readily available in health care facilities. It uses metal electrodes attached to the extremities and chest wall to measure electric potential, which is then visualized by the ECG machine.
Reference
This discussion is based on Dr. Edgar M. Rotairo’s presentation and Dr. Ferrer’s live lecture.
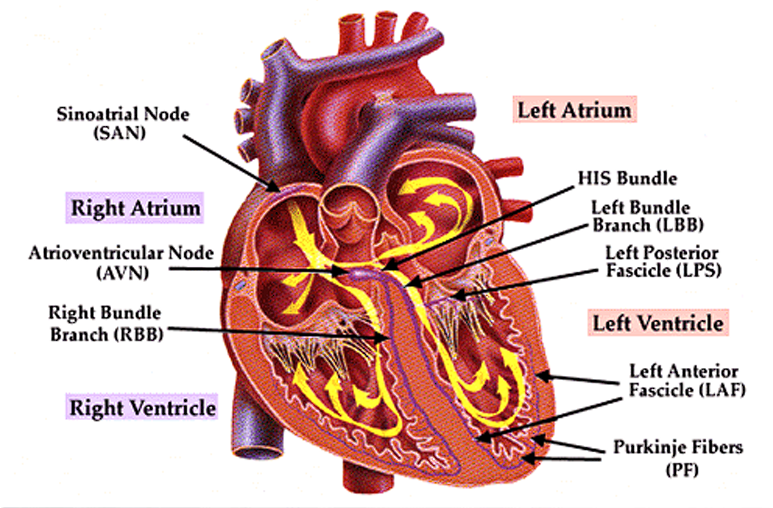
Conduction System of the Heart
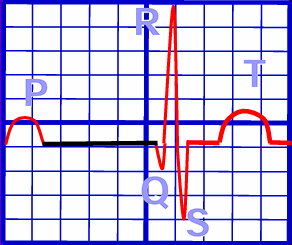
- In normal physiology, the electrical impulse originates from the sinoatrial node, depolarizing the right atrium, being recorded as a P wave.
- The impulse travels down to the atrioventricular node,
- The Bundle of His continues the impulse, splitting into the right and left bundle branches.
- Finally, the Purkinje Fibers are predominant carriers of impulse within the ventricles, travelling downward, turning at the apex of the heart to wrap around the myocardium upwards. The resulting ventricular contraction is seen as the QRS Complex.
- Finally, the T wave is a sign of ventricular repolarization.
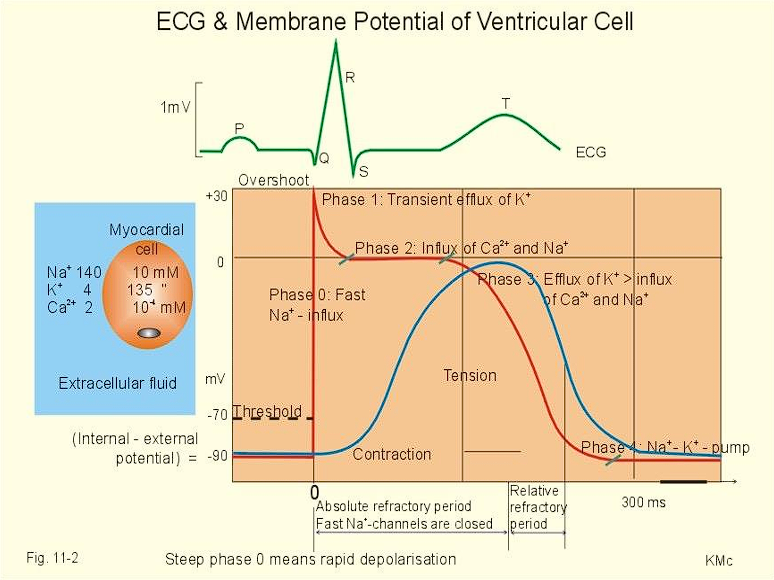
Depolarization-Repolarization Cycle
| Phase | Electrolyte Flow |
|---|---|
| Phase 0: Rapid Depolarization | Sodium rapidly enters cardiac cells |
| Calcium slowly enters cardiac cells | |
| Phase 1: Early Repolarization | Sodium channels close |
| Potassium temporarily increases from efflux | |
| Phase 2: Plateau Phase | Calcium continues to flow in |
| Potassium continues to flow out | |
| Phase 3: Rapid Repolarization | Potassium channels open, rapid diffusion |
| Calcium channels become inactivated | |
| Phase 4: Resting Phase | Sodium-Potassium pump returns Na and K to their states. |
| Cell membranes become impermeable to sodium ions. |
Lead Placement
The following are the corresponding leads to which wall of the heart is being detected:
- II, III, AVF: inferior wall
- I, AVL: lateral wall
- V1, V2: septal wall
- V3, V4: anterior wall
- V5, V6: lateral wall
- AVR: no specific view
Coronary Artery Sources
- The Right Coronary Artery supplies the inferior wall.
- The Left Coronary Artery supplies the anterior, septal, and lateral walls.
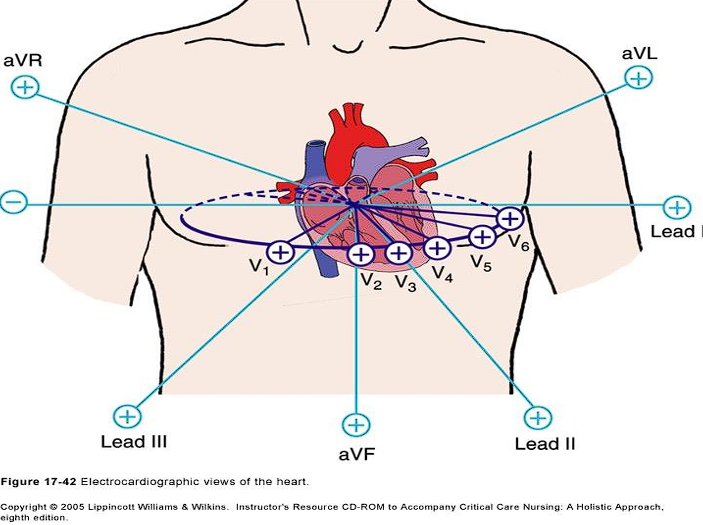
Unipolar Precordial Leads
- V₁: 4th ICS, Right Sternal Margin
- V₂: 4th ICS, Left Sternal Margin
- V₃: Midway between V₂ and V₄
- V₄: 5th ICS, MCL
- V₅: AAL on the same level as V₄
- V₆: MAL on the same level as V₄

Lead Axes
The two leads to consider for axis deviation is Lead I and Lead AVF. If both are positive, the axis remains normal.
| Lead I | Lead AVF | Axis |
|---|---|---|
| Positive | Positive | Normal |
| Positive | Negative | Left |
| Negative | Positive | Right |
| Negative | Negative | Extreme Axis Deviation |
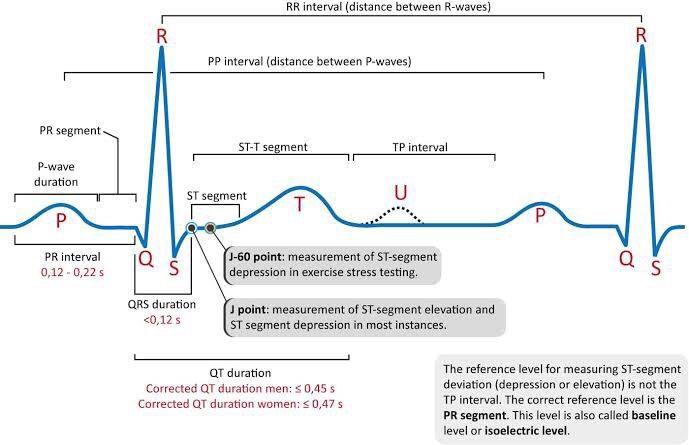
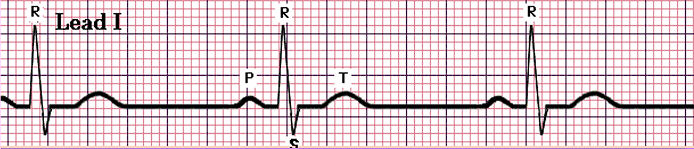
ECG Wave Parameters
An electrocardiograph is an axis of time (0.04s per cell) and electrical potential (inc). These cells are grouped into a five by five larger square, spanning 200 milliseconds.
- P Wave: atrial depolarization; the duration of atrial conduction. Normally 0.5 to 2.5 mm in amplitude when graphed, and up to 0.10s in duration in adults.
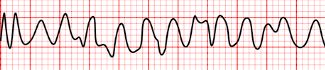
- Rapid sequence of P waves (sawtooth appearance) indicate atrial flutter, as the atrium rapidly depolarizes.
- Absence of P waves is termed atrial fibrillation, when the heart fails to establish meaningful contractions, and instead wiggles in place.
- PR Interval: significant duration for detecting heart block, as it is the period of time for impulses to travel from the SA node to the ventricles. It is measured in limb leads with the longest PR. Normally 0.12 to 0.20 s in adults, equivalent to 70 to 90 BPM.
- QRS Complex: ventricular depolarization. Normally 0.06 to 0.10 s, at least less than 0.12 s.
- QT Interval: Normally less than 0.44 s.
- A prolonged QT interval can also result from heart block.
- ST Segment: the period from the end of ventricular depolarization to ventricular repolarization.
- ST segment elevation is a characteristic finding for myocardial infarction.
- ST segment depression is a sign of myocardial ischemia.
- T Wave: ventricular repolarization
Reading ECGs
There are multiple parameters that an ECG reading depends on. These include the Rate, the actual heart rate of the patient; Pattern, QRS Complexes; P Waves; and the P-QRS Complex Relationship.
Heart Rate Calculation
The formula or can be used to determine the heart rate of an individual from an ECG reading.
- Sinus Rhythm: the normal rhythm, with a P wave followed by QRST with no narrowing or widening. The normal heart rate is dictated by the sinus (SA) node, the heart’s primary pacemaker. In an adult, the resting heart rate ranges from 60 – 100 beats/min.
- Sinus Bradycardia: a normal waveform but with a slow heart rate, less than 60 beats/min.
- Sinus Tachycardia: a normal waveform but with a fast heart rate, more than 100 beats/min.

- Sinus Arrhythmia: a normal waveform occurring in irregular intervals; with the longest PP interval or RR interval being larger by the shortest by 0.16 seconds or more.
- Premature Atrial Complex: a prematurely occurring PQRST complex. The P wave appears outside of the normal sinus beat, resulting in a long PR interval and a narrow QRS complex.
- Atrial Flutter: an atrial rate of 220 to 300 beats/min, with only the P section of the waveform (atrial depolarization) appearing as flutter waves.
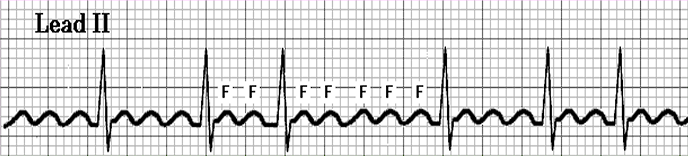
- Atrial Fibrillation: the atrium is rapidly triggered, resulting in no discernible P waves, with an irregular RR interval.

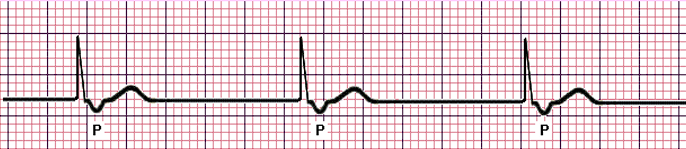
- Junctional Rhythm: once the primary pacemaker (SA node) fails to lead the heart’s impulses, the AV Node takes over, but produces a lower normal heart rate. The P wave becomes inverted or buried within or follows the QRS complex, and the QRS complex itself is narrow.
- Premature Ventricular Complex: a prematurely occurring complex; the QRS complex ends up looking wide and bizarre, with no preceding P wave. The following T wave becomes inverted in defection to the QRS complex. After each PVC, a compensatory pause occurs for the heart to reorient its signals.
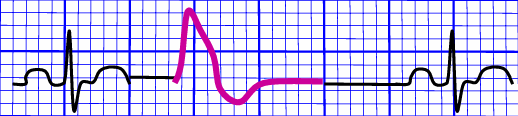
- Ventricular Tachycardia: a series of at least three consecutive PVCs that display rapid, bizarre, wide QRS complexes (>0.10s). As previously mentioned, PVCs do not have a preceding P wave, which normally act as the origin of ventricular impulses.
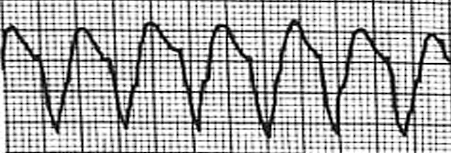
- Ventricular Fibrillation: the complete loss of discernible P, QRS, and ST segments as the ventricle loses its ability to contract as a unit. This is the most common mechanism of cardiac arrest in myocardial ischemia and infarction.
Heart Blocks
Atrioventricular blocks are a dysfunction of the conductive system of the heart where the time between the activation of the atrium and the ventricles (PR segment) become prolonged.
-
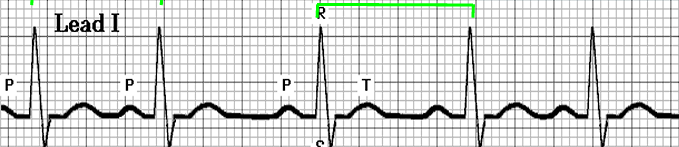
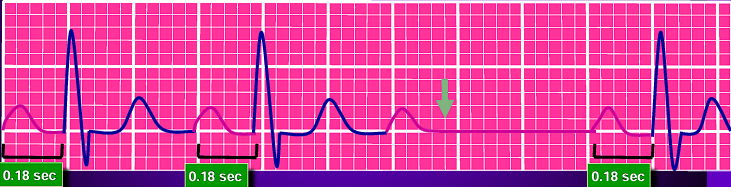
First Degree Atrioventricular Blocks: a prolonged PR interval (>0.2s). The impulse continues as normal, hence this often appears asymptomatically and does not require treatment.
-
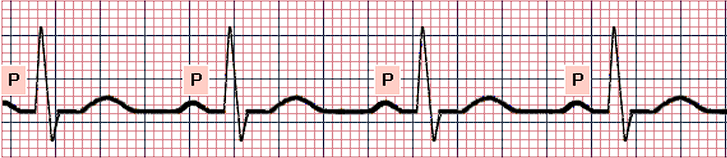
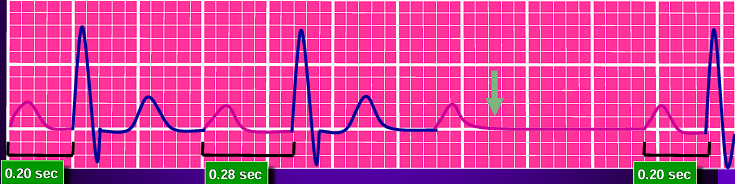
Type 1 (Mobitz I or Wenckebach) Second Degree Atrioventricular Blocks: a series of progressively lengthening PR intervals, until eventually a QRS complex is dropped (P wave not followed by QRS). This is a cyclic process that is often benign and may not require treatment.
-
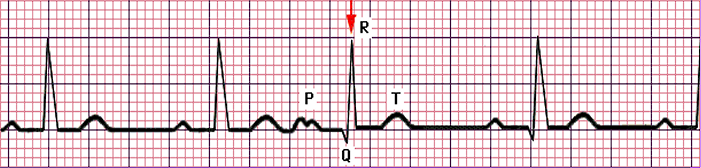
Type 2 (Mobitz II) Second Degree Atrioventricular Blocks: a stable PR interval with intermittently dropped beats (missing QRS complex).
-
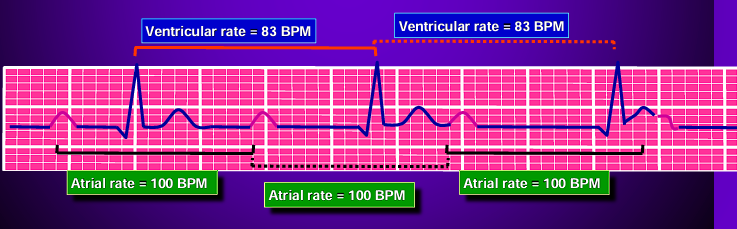
Third Degree Atrioventricular Blocks: a “complete heart block” where atrial and ventricular activity are completely detached from one another. The QRS complexes often become abnormal in shape, duration, and axis. They maintain a constant rate and morphology.
Antiarrhythmic Medications
| Class | Action | Examples | Side Effects |
|---|---|---|---|
| 1A | Fast sodium channel blocker varies depolarization and action potential duration | Quinidine Procainamide Disopyramide | Class: nausea, vomiting Quinidine: hemolytic anemia, thrombocytopenia, tinnitus Procainamide: lupus |
| 1B | Lodicaine Mexiletine | Lidocaine: dizziness, confusion, seizures, coma Mexiletine: tremor, ataxia, rash | |
| 1C | Flecainide Propafenone | Flecainide: pro-arrhythmia, nausea, dizziness | |
| 2 | Beta-blockers: decreasing SA node and AV node conduction. | Propanolol Metoprolol | Class: CHF, bronchospasm, bradycardia, hypotension |
| 3 | Prolong action potentials by blocking K+ channels | Amiodarone Sotalol | Amiodarone: hepatitis, pulmonary fibrosis, thyroid disorders, peripheral neuropathy Sotalol: bronchospasm |
| 4 | Calcium Channel Blockers: decreasing AV node conduction | Verapamil Dilitiazem | Class: AB block, hypotension, bradycardia, constipation |