Updated on Oct. 16, 2024, expanding on Preoperative Medications, Sedation, Hemostasis, Postoperative Discomforts, and Postoperative Complications
This page is lifted from Sir V’s handout on Perioperative Nursing and supplemented with information from live lectures. I also added information when appropriate to provide more context.
When I have time, full lectures on perioperative nursing will be linked here. The sources I have for perioperative nursing are all pretty long, so they will have to wait.
Perioperative Nursing
Perioperative nursing is the identification of the physiological, psychological, social and spiritual needs of the client and the formulation of an individualized plan of care before, during, and after surgery. Surgeries are done to cure, to relieve pain, to prolong life, to maintain dynamic body equilibrium, to treat and prevent infection, or to correct deformities or defects. For this vast array of functions, surgeries take on various forms:
| Classification | Types |
|---|---|
| According to Purpose | Curative: to repair or remove damaged tissue to cure disease Diagnostic: to verify or establish a diagnosis Exploratory: to explore the extent of disease or damage Ablative: to remove non-functional tissue Palliative: to reduce symptoms, without curing the disease process Transplant: to transfer organs |
| According to Location | External, e.g., a hysterectomy Internal, e.g., skin grafting |
| According to Mode | Constructive: to create structures, especially in congenital defects Reconstructive: to restore structures |
| According to Degree of Risk | Minor: non-life-threatening procedures Major: involves vital signs or vasculature, or with the potential for bleeding. Factors: duration, expected blood loss, organs involved, type of anesthesia, age of patient, degree of trauma |
| According to Urgency | Emergency: immediately required procedures done within 24 hours. Urgent: procedures that must be done within 48 hours. Elective: may still be required, but can be scheduled within days to months. |
Pathologic Conditions
There are four basic pathologic conditions that require surgery: obstruction, such as in a blocked bile duct; perforation, the rupture of an organ, artery, or bleb i.e. in aneurysms; erosion, a break in the continuity of tissue surfaces caused by irritation, infection, ulceration, or inflammation; and tumors, abnormal growths of tissue that serve no physiologic function in the body.
The Surgical Team
The medical team handling an patient in the operating room is composed to a multidisciplinary set of members that all play their respective roles for providing holistic care. They are generally divided between sterile and unsterile members of the team:
| Team | Members |
|---|---|
| Sterile | 1. Operating Surgeon 2. Assisting Surgeons 3. Scrub Nurse |
| Unsterile | 4. Anesthesiologist 5. Circulating Nurse 6. Adjunct Personnel |
Scrub Nurse
The scrub nurse is a sterile member, and assists the surgeon during the operation by providing sterile instruments and supplies, counting instruments, or sometimes even basic functions of assistant surgeons such as retracting, suctioning, and assisting in suturing (sponging, cutting).
- Receives patient from the surgical ward nurse (if circu is busy).
- Prepares and organizes the OR unit based on the case. (Another source says circulating nurses does this 1 hour prior to incision time).
- Back table
- Mayo table
- Extra table
- OR Table + attachments (arm board, foot board, straps, anesthetic monitor, anesthesia screen, donut to prevent head from moving)
- Equipment for anesthesia, IV
- Spinal set
- Skin preparation set
- Opens sterile packs and adds sterile supplies and instruments.
- Performs surgical scrubbing, gowning, and (closed) gloving. Before doing so, the prerequisites include:
- OR attire (scrub suit, shoes, mask, cap), rolled sleeves if long
- Skin integrity, short fingernails, no nail polish, no jewelry
- No persistent cough
- Organizes sterile fields and maintains its integrity, safety, and efficiency.
- Serves gowns and gloves to surgeons
- Counting of instruments
- Draping
- Mayo Cover, Mayo Towel
- 4 OR Towels used to outline the operative site, on the left, right, top, and bottom margins. These are secured with towel clips.
- Foot Drape
- Lap Sheet, a sheet with a fenestration (hole) that is aligned with the surgical site.
- Announcing cutting time.
Circulating Nurse
The circulating nurse provides assistance to any member of the OR team in any manner they are qualified for. Circulating nurses are crucial in communication, direction, and safety.
- Receives patient from the surgical ward nurse. Endorsement during transfer includes confirmation of patient identity, schedule, and securing informed consent. Discussed later: Preoperative Preparation
- Establishes rapport with the client.
- Places the patient on the OR table and remains with them.
- Position the patient for anesthesia. This may be supine or quasi-fetal position depending on the anesthesia being used. Relative to the patient, the nurse maintains the fetal position by holding their knees and nape from in front of the patient.
- Perform lumbar preparation for spinal or epidural anesthesia. The solution used is directly 10% Betadine.
- Catheterize the patient if necessary. For women, use the dorsal recumbent position. For men, supine is sufficient.
- Skin preparation. The area prepared must be larger than the area bring operated on. For example, the skin prep for a caesarean section starts from the nipple line to the knees. The umbilicus then abdomen is cleaned thrice, and the legs are also cleaned thrice.
- Position the patient for surgery.
- Help drape the patient.
- Handle, label, and send tissue samples for analysis.
- Record starting time, cutting time, closing time, etc. After cutting time, the circulating nurse mainly handles charting and charging (counting used instruments and other equipment).
Others
- Operating Surgeon: pre-operative diagnosis and care; actual performance of operation; post-operative management and care. They assume full responsibility as the “captain of the ship”, providing all medical acts of judgment and management.
- Assisting Surgeons: those who hold retractors, clamps bleeders, assists in sutures (especially for closure), and suctioning. These individuals may be physicians, non-physicians (clerks, interns, etc.), registered nurse first assistants (RNFA), or well-experienced OR nurses.
- Anesthesiologist: administers and maintains anesthesia and manages untoward reactions to anesthesia.
- Adjunct Personnel: additional specialists that may enter as unsterile members of indicated, e.g., a neonatologist for a premature baby born via C.S.
Surgical Landmarks and Positioning
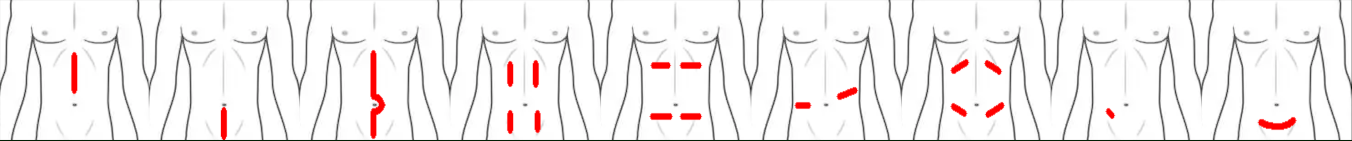
Many landmarks and subdivisions are used in surgery, used appropriately depending on the purpose of the surgery. Surgical incisions include:
- Upper Midline Incision: midline incision above the umbilicus
- Lower Midline Incision: midline incision below the umbilicus
- Longitudinal Midline Incision: midline incision above, around, and below the umbilicus. Not through the umbilicus directly. This is the longest incision on the abdominal surface.
- Paramedian Incision: meaning “adjacent to the midline”. It is a longitudinal incision performed in one or more of the four quadrants of the abdomen.
- Mid-abdominal Transverse Incisions: same as paramedian incisions, but perpendicular to the long axis of the body.
- Thoracolumbar Incisions: an incision perpendicular to the long axis of the body. This incision may be flat or oblique, and extends to the back. The incision is aligned with the kidney, and is used for nephrectomy.
- Oblique Incisions: incisions similar to paramedian incisions, but at oblique angles. These may also be called as subcostal (upper oblique) incisions, or inguinal (lower oblique) incisions.
- McBurney’s Incisions: an incision at McBurney’s point, the midpoint between the umbilicus and the right anterosuperior iliac spine. This is used to locate the position of the appendix, and is the most common site of maximum tenderness in acute appendicitis. However, in ruptured appendicitis, a right lower paramedian incision is used for exploration and lavage.
- Pfannenstiel Incisions: the most common method for performing caesarian sections in present day. It is a slightly curved transverse incision between the symphysis pubis and umbilicus.
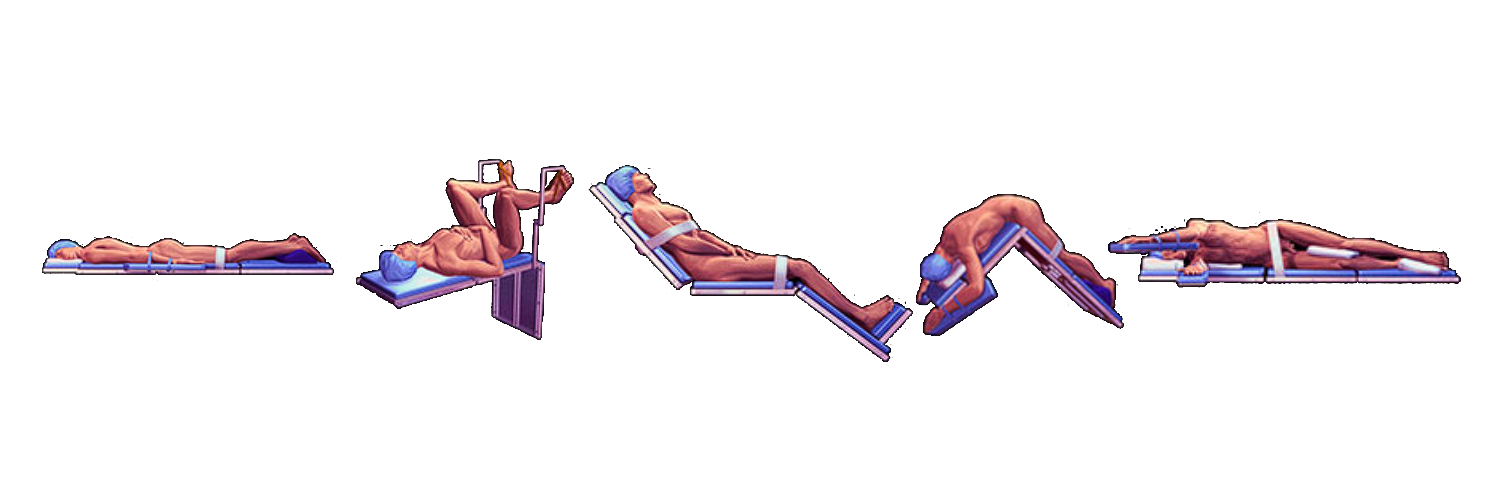
The patient is positioned in whichever position is most ideal for the area being operated on for both the surgeon (access and view of surgical site) and anesthesiologist (no pressure on major blood vessels and will not impede circulation). This includes:
- Supine Position, also known as the Dorsal position.
- Prone Position: the patient lies on their stomach with their head turned to one side. This is used for spinal, rectal, or perianal procedures. It can lose problems with respiration, making it one of the more difficult positions.
- Lithotomy Position: the patient is supine with their hips and knees flexed, with the legs elevated and supported by stirrups. This is used for gynecological, urological, and colorectal procedures.
- Semi-Fowler’s/Fowler’s Position: supine, with the head of the bed elevated at 30° to 45°. This is used for head, neck, or chest procedures e.g. CTT, Paracentesis, bronchoscopy
- Kraske/Jackknife Position: the patient is positioned prone, with the operating table set to flex at the hip. This elevates the pelvis above the rest of the body. This is used for rectal (e.g. hemorrhoidectomy) and some spinal procedures.
- Lateral Position: the patient is positioned on their side (side-lying). This is used for thoracic, renal, and hip procedures. Proper padding and positioning aids is required for proper alignment and stability. This is used for endoscopy, bronchoscopy, and colonoscopy
- Trendelenburg Position: a normal supine position, with the head of the bed lowered and foot of the bed raised. The body maintains a neutral and straight posture. This is rarely used as the position impairs breathing from the abdominal organs placing pressure on the diaphragm. This is normally temporarily used to locate organs.
- Reverse Trendelenburg Position: the Trendelenburg position with the head elevated. Used for nose and neck surgery to avoid aspiration.
- Kidney Position: an amalgamation of the jackknife position and the lateral position. The patient is side-lying, bent at the level of the kidney (around the costovertebral angle) to make it protrude above the rest of the body. By naming convention, this is labeled as left or right kidney based on which kidney is exposed, i.e., right kidney position exposes the right kidney, and is equivalent to the left lateral jackknife position.
The abdominal cavity is occupied by many organs of the gastrointestinal system, renal system, reproductive systems (females), etc. There are two general subdivisions of the abdomen:
- Nine-Region System: this system divides the abdomen into nine areas using two horizontal and two vertical lines (midclavicular lines). The lowest region ends at the level of the highest part of the pelvic bone (transtubercular line), and the highest region ends at the end of the ribcage (subcostal line).
| Left | Middle | Right |
|---|---|---|
| Left Hypochondriac | Epigastric | Right Hypochondriac |
| Left Lumbar | Umbilical | Right Lumbar |
| Left Iliac (Inguinal) | Hypogastric (Suprapubic) | Right Iliac (Inguinal) |
- Four-Quadrant System: this system divides the abdomen into four with the midline from the xiphoid to the symphysis pubis, and a transverse cut across the umbilicus.
| Left | Right |
|---|---|
| Left Upper Quadrant | Right Upper Quadrant |
| Left Lower Quadrant | Right Lower Quadrant |
Preoperative Phase
The patient has to undergo preparations prior to surgery, with some requiring preparation days or weeks prior to surgery. Generally, these are the preoperative preparations to perform the day and night before the surgery:
- Pre-operative visit the day before the surgery.
- Client education on post-operative activities, such as breathing exercises to avoid pulmonary atelectasis, splinting coughs, etc.
- Complete laboratory and diagnostic examination coordinated with the MD.
- Cardiopulmonary (CP) Clearance: an initial evaluation to determine if the patient will be able to undergo surgical intervention on general anesthesia. Not being cleared indicates an elevated risk for cardiac events during surgery.
- Checking of blood products when indicated.
- Monitoring VS and I&O.
- Secure consent.
- Bathing as necessary.
- Light evening meal and NPO from midnight to the time of the surgery. No oral intake should be had to prevent emesis and pulmonary aspiration of gastric contents when placed under general anesthesia. Failure to maintain NPO status can be grounds for delaying surgery.
- Psychological and spiritual support.
- Administration of laxatives if indicated.
- Removal of nail polish (for accurate pulse oximetry).
On the morning of the surgery itself, the most important nursing actions include:
- Ensuring NPO for reasons previously mentioned.
- Oral care.
- Enema if ordered.
- Shaving areas to be operated on.
- Reviewing post-op exercises like those previously mentioned.
- Preoperative medications are also given at this time. They are discussed later in this section.
- Monitoring of patient status, including their psychological state. Provide support as necessary.
- Removal of dentures as aspiration precautions, jewelry, wigs, prosthetics(of possible), etc.
- Endorsement to the OR from the surgical ward.
Pre-operative medications are given to prepare the client for anesthesia and potentiate its effects, and to sedate the client to reduce anxiety levels. The anesthesiologist prepares the cocktail and the medication is given to the patient at least 30 to 60 minutes before the surgery. These include:
- Narcotic Analgesia: nubain (least potent), demerol, morphine (most potent)
- Sedatives: often phenergen
- Anticholinergics: to reduce the production of secretions. A common example is atrophine sulfate.
Consent
Informed Consent is a condition of understanding and willingness to undergo a procedure. The distinction of “Informed” specifies that the patient understands all pertinent information related to the procedure, such as purpose, risks, benefits, alternatives, side effects, cost, among others. For this, the patient is required to be of sound mind and of age.
Also read: Consent in Health Care
Intraoperative Phase
The intraoperative phase includes the goals of care of asepsis, infection control, homeostasis, safe administration of anesthesia, and hemostasis.
Asepsis
Asepsis, disinfection, and sterilization are all varying ways to reduce or completely eliminate the presence of microorganisms on a field or body to produce an environment viable for surgical procedure.
- Asepsis: the elimination of microorganisms from living tissue. Medical asepsis (clean technique) limits microorganisms, while surgical asepsis (sterile technique) eliminates all microorganisms.
- Disinfection: the elimination of microorganisms from inanimate objects, excluding spores.
- This may be done through physical or chemical methods. Physical methods include boiling (5 to 10 minutes), steaming, and sunlight. Chemical methods include alcohol, chlorine, iodine, and phenol (esp. for AP).
- Sterilization: the elimination of microorganisms from inanimate objects, including spores.
- This may be done through physical or chemical methods. Physical methods include autoclaving, the main method of sterilization, radiation, and gas (ethylene oxide; ETO). Chemical methods mainly involve soaking/immersion.
Autoclave Sterility
In storage, packed autoclaved items can remain sterile for up to 28 days in a closed shelf, and up to 21 days on an open shelf.
- Packing materials: linen (muslin), paper, or plastic. The most ideal material for use is plastic.
| Solution | Sterilization | High Level Disinfection | Intermediate Level Disinfection | Low Level Disinfection | Notes |
|---|---|---|---|---|---|
| Cidex Activated | 10 hours | 45 mins | 15 to 45 mins | 5 to 15 mins | Solution only used for 14 to 30 days |
| Cidex OPA (0.55%) | - | 12 mins | - | - | Solution only used for 14 days |
| Cidex OPA (5.75%) | 32 hours | 5 mins | - | -Intermediate Level | Used for automatic endoscopic high level disinfection |
- Low Level Disinfection: kills fungi and viruses
- Intermediate Level Disinfection: kills fungi, viruses, and bacteria
- High Level Disinfection: kills all microorganisms except spores
- Sterilization: kills all microorganisms including spores
Earle Spaulding created the Spaulding Classification to determine the level of disinfection required for items being used for
- Critical: used for items that cut into intact skin and mucous membranes or items entering vascular areas of the body. This requires sterilization.
- Semi-Critical: used for items coming into contact with non-intact skin and mucous membranes. This requires high-level disinfection.
- Non-Critical: used for items coming into contact with intact skin and mucous membranes. This requires intermediate-level to low-level disinfection.
Principles of Sterile Technique
- Only sterile items are used within the sterile field. If in doubt of integrity, consider an item unsterile.
- Sterile personnel are gowned and gloved. Gowns are only sterile from the level of the shoulder to the waist. The back is considered unsterile. The sleeves are only considered sterile up to two inches above the elbow.
- Tables are sterile only at table level. The level of the table should not be changed too frequently.
- Sterile personnel touch only sterile items or areas; unsterile personnel touch only unsterile items or areas.
- Unsterile personnel avoid reaching over the sterile field and sterile personnel avoid leaning over an unsterile area.
- The edges of anything that encloses sterile contents are considered unsterile.
- The sterile field is created as close as possible to the time of use, and kept as dry as possible.
- Sterile areas are continuously kept in view. Overt contamination of the sterile area is better than covert contamination.
- Sterile personnel keep well within the sterile area.
- Sterile personnel keep contact with sterile areas to a minimum.
- Destruction of the integrity of microbial barriers results in contamination.
- Microorganisms must be kept to an irreducible minimum.
Surgical Scrubbing
| Time Method | 1st (5 min.) | 2nd (4 min.) | 3rd (1 min.) |
|---|---|---|---|
| Hand | 1 minute | 1 minute | 30 seconds |
| Arm | 1 minute | 1 minute | None |
| Elbow | 30 seconds | None | None |
| Brush-Stroke Method | 1st (5 min.) | 2nd (4 min.) | 3rd (1 min.) |
|---|---|---|---|
| Fingertips | 10, 3 (sides of fingers) | 5, 3 (sides of fingers) | 3 |
| Hand | 10 | 5 | 3 |
| Arm | 6 | 3 | 0 |
| Elbow | 6 | 0 | 0 |
Surgical Instrumentation
Instruments used during surgeries are generally divided between sharps to cut, graspers to hold, clamps to occlude, and retractors to reveal.
I really can’t be bothered to add images for all of these. Use Google if you’re not familiar with them.
Sharps
Equipment used for cutting, dissecting, or piercing tissues.
- Knives: the primary cutting tool for membranes. These come in differing sizes for varying tissues. Blades from 20 to 25 are paired with handle #4, and is used to cut tough tissues (skin, fascia layers; tendons, ligaments, and bones). Blades from 10 to 15 are paired with handle #3, and is used to cut delicate tissues (subcutaneous, muscular, peritoneum layers; uterus).
- Handles: the handle for knives. These are either #4 for blades 20, 21, 22, 23 and 25, or #3 for blades 10, 11, 12, 13, and 15.
- Only when a knife is placed on a handle is a scalpel formed.
- Scissors:
- Curved Mayo Scissors: used for heavy or tough tissues.
- Metzenbaum (Metz) Scissors: used for delicate tissues.
- Straight Scissors: used for cutting sutures.
- Bandage Scissors: cutting tough tissues, particularly the uterus and the umbilical cord during caesarean section.
- Steven’s Scissors: cutting off eyelashes
- Needles: straight or curved (cutting or round) needles used for puncturing the skin to create stitches. These are paired with ties for suturing.
- Sutures are surgical-use threads used for closing wounds/creating stitches. They may be absorbable (dissolves by itself within the body), or non-absorbable.
| Absorbable Sutures | Synthesis | Description | Absorption | Handling Char. |
|---|---|---|---|---|
| Catgut (Chromic) | Non-synthetic | Brown; used in all tissue except subcutaneous layer | 90 days | Do not soak |
| Catgut (Plain) | Non-synthetic | Light Yellow; used for subcutaneous layer | 70 days | Do not soak |
| Dexon | Synthetic | Green | 90 days | Do not wet |
| Vicryl | Synthetic | Violet | 120 days | Do not wet |
| Non-absorbable Sutures | Synthesis | Description | Handling Char. |
|---|---|---|---|
| Silk | Non-synthetic | Appears black, actually navy blue | Do not wet |
| Cotton | Non-synthetic | Appears white, actually light pink | Should be wet |
| Nylon | Synthetic | Black or blue. Despite its category, nylon is actually absorbed in four years (25% per year). | Can be wet |
Suture Sizing
Sutures are sized by number, with the largest being
1. Appendage of-0i.e.1-0makes it smaller. The next smaller size is2, and so on.
Graspers
“Grasps” tissues. They hold tissue of the patient.
- Thumb Forceps: used to hold delicate tissues. The tip of these are toothless.
- Tissue Forceps: visually the same as thumb forceps, but feature a tooth at the end of the forceps.
- Babcock Forceps: forceps with a cylindrical cavity used to handle tubular, delicate tissues.
- Allis Forceps: toothed, rake-like forceps used for tougher tissues like bones, tendons, and fascia.
- Adson Forceps: toothed forceps used for tougher tissues.
- Pennington Forceps: triangular forceps used for perineal or rectal surgery.
- Ovum Forceps: used for delicate forceps. These are also used as pick-up forceps.
The sharps, graspers, and needles are classified according to their use for you or delicate tissue. When working on their respective tissues, they are paired accordingly. When dissecting, the sharps and graspers are used. When suturing, the graspers and needles are used.
| Class | Sharps | Graspers | Needles |
|---|---|---|---|
| Tough | Mayo | Allis Tissue | Cutting |
| Delicate | Metz | Thumb Babcock Kelly | Round |
Clamps
Tools used for occluding vessels or to produce hemostasis. Each of these have straight and curved variants.
- Mosquito: the shortest clamp; used for minor surgery, pediatrics, and handling superficial layers.
- Crile: medium-sized; used for shallow layers.
- Kelly: the longest; used for abdominal layers or cavities.
- Ochsner: strong, fully-serrated clamp with a tooth at the end that crushes tissue to prevent bleeding. It is commonly used for hysterectomies.
- Mixter: a forcep that curves at the end, used to maneuver around structures to reach hard places.
Retractors
These are exposing instruments. These are further specified as self-retaining (does not require manual application of force) or non-self-retaining (requires handling).
Self-Retaining
- Balfour Abdominal Retractor: a large self-retaining retractor primarily used in abdominal surgeries. Two lateral blades and a central blade can be adjusted to keep the abdominal wall open.
- Weitlaner Retractor: a small self-retaining retractor with two arms ending in outward-pointing, curved prongs. This is used for a thyroidectomy.
- Mastoid Self-Retaining Retractor: a scissor-like tool with rake-like ends used for small operative areas.
- Gelpi: a scissor-like tool with pointed tips used for perineal surgery.
Non-Self-Retaining
- Army Navy Retractor: a double-edged handheld retractor with a straight handle and two blades of different lengths on each end. These are used for superficial layers.
- Richardson Retractor: a single or double-ended handheld retractor with a right-angled blade. It is a curved, concave blade that comes in different sizes.
- Deaver Retractor: a long, flat handheld retractor with a scoop-like blade at one end. It often holds back large organs like the liver or intestines, providing exposure to deep areas of the abdominal cavity.
- Bladder Retractor: a specialized handheld retractor that gently moves and holds the bladder or other pelvic organs away from the surgical site.
- Murphy/Rake Retractor: a rake-like retractor with varying number of teeth.
- Senn Retractor: also a rake-like retractor, used for superficial/skin retraction. It can be double-ended, or have one end that is curved and concave.
- Malleable/Ribbon Retractor: a softer retractor that can be shaped as necessary.
Sedation
Anesthesia is the loss of sensibility to pain. In administration, there are four stages of anesthesia:
- Induction: the preparatory phase of anesthesia; the patient feels drowsy or dizzy. Sensation of pain begins to dull.
- Excitement: breathing becomes irregular, and involuntary motor movements may appear. This may be viewed as the patient struggling. This appears as the patient loses sensation in the anesthetized region.
- Surgical Anesthesia: the period appropriate for surgery when pain is no longer felt; muscles are relaxed, pupils are constricted, and the pupil reflex is absent.
- Medullary Depression: oversedation/overdose; depression of the medulla oblongata, which can cause respiratory cessation and potentially death.
Signs of Complication
Cyanosis. At Time Out, the patient’s fingers (nail beds), and face (lips) are checked for cyanosis, which can act as a result of respiratory compromise. Spontaneous breathing is checked (disable the anesthetic ventilator).
Furthermore, if CPR is required, the scrub nurse prioritizes the sterility of the mayo and back table. The circulating nurse and assistant surgeon perform CPR and prepare medications. Afterwards, the surgery can be continued after re-draping and re-gowning.
Depending on the scope of the anesthesia, it can be considered as general anesthesia (IV, inhalation) that produces sensory, motor, reflex, and mental blocks; or anesthesia that only affects one area of the body— regional anesthesia (spinal, epidural, nerve blocks, infiltration, application, spray). The following are commonly used anesthetics (I’ve highlighted the ones mentioned during the review):
- Non-Halogenated Inhalants: gas delivered through an ET/mask
- Nitrous Oxide (Blue) used for initial restlessness. This is the most common inhaled gas.
- Cyclopropane (Orange) used for short procedures
- Halogenated Fluid/Liquid Inhalants:
- Halothane (Red) used for hypotension
- Forane
- Ethrane
- Enflurane (Yellow) used for muscle relaxation
- Sevoflurane (Sweet-tasting) used for pediatric patients
ET Sizing is approximately the same diameter as the patient's pinky finger.
The insertion of an ET utilizes a laryngoscope for guidance. When meeting the esophagus, Sellick’s Maneuver is used to depress the cartilage for the esophagus. In nurses, training is required to be able to perform this task.
- Intravenous Barbiturates: Thiopental Sodium (Sodium Penthotal), Ketamine (Ketalar)
- Neuroleptic Agents: Fentanyl, which decreases motor activity
- Dissociative Agents: Ketamine, which can cause hallucinations
Local anesthesia is a class of regional anesthesia which function at a narrower scope than even regional anesthesia. These are applied through injection, spray, or topical application. These do not produce a change in the level of consciousness. These also take on different forms:
- Topical: applied over the surgical site, e.g.:
- Prilocaine (Euthetic Mixture of Local Anesthesia [EMLA] Cream)
- Xylocaine (via syringe or spray)
- Lidocaine
- Lignocaine
- Field/Nerve Block: injected into subcutaneous or perineural spaces near or around the desired anesthesia site, blocking pain impulses from passing through plexuses (“main terminals of pain”). Examples of this include brachial plexus block for the upper extremities, “Saddle Block” for the sacral/perineal area.
- Spinal: anesthesia injected intrathecally directly into the subarachnoid space (inside the arachnoid). Contrastingly, this affects both sensory and motor function, while epidural does not block motor function. The needle used is long and large-bore.
- Epidural: anesthesia injected intrathecally into the epidural space (outside of the arachnoid), commonly used in obstetrics. Motor function is not blocked, hence this is used for delivery to maintain uterine contractions while blocking pain. The syringe used is short but large-bore, containing a passageway to be used for administration.
- Anesthetic agents (also for spinal) include: sensorcaine, bupivacaine, pontocaine, and tetracaine.
Spinal and Epidural Administration
- The vertebral bones are made prominent by the quasi-fetal position of the patient. This is injected between L3 and L4, which targets the lower abdomen. If the space that receives anesthesia is higher (e.g. L1, L2), the diaphragm may become affected, which results in respiratory arrest.
- Post-operatively, the patient is laid flat without a pillow to avoid a spinal headache. They are weaned into an upright angle to prevent dizziness and vomiting.
Hemostasis
Hemostasis is the cessation of hemorrhaging from an injured blood vessel. In a normal wound, this occurs in three stages: vasoconstriction, platelet plug formation, and coagulation. However, in a surgery, artificial methods can be used to induce hemostasis:
- Mechanical:
- Pressure via manual or digital pressure
- Suture (free tie, stick tie, SutLig) for ligation or suturing. The sutlig, short for suture-ligature, consists of a line, needle, and needle holder. The needle used may be of two types: (1) eyed needle, which is atraumatic and reusable; and (2) eyeless needle, which may be single-armed, or double-armed depending on the number of needles connected to the line.
- Dressing
- Clamping
- Gel Foam: used for light bleeders that make it past suturing in the abdominal layers. The foam covers and absorbs the blood that leaks, which then swells and produces pressure to stop the bleeder. This is made of protein, and is absorbable within one month.
- Drains (Penrose drain) do not directly stop bleeding, but stops further trauma or infection.
- Chemical: tissue adhesion
- Coagulant medications, most commonly tranexamic acid (Hemostan) for surgical use.
- Oxytocic drugs prevent postpartum uterine atony and subsequent bleeding by enhancing uterine contraction.
- Bone wax, a wax-like substance that is rubbed onto bleeding bone tissue to attempt to stop bleeding, especially during open reduction.
- Thermal:
- Heat: electrocautery, the use of a cautery line (tool used by surgeon) and a ground (pad placed under the patient with KY jelly)
- Cold: liquid nitrogen used in cryosurgery, a surgery where the site of surgery is frozen.
Nursing Activities
Watch for bleeders; the nurse may remind the surgeon to use hemostasis if any bleeders are present.
Postoperative Phase
Immediate Care
This is care provided while the patient remains in the recovery room.
- Assure ABCs:
- O₂ therapy with positioning, artificial airways until the return of gag reflex, suctioning, encouraging deep breathing
- Check vital signs every 15 minutes until stable, then every 30 minutes.
- Check skin color, temperature, drainage, and dressings. These are among the overt signs of infection or failing circulation, among other complications.
- Monitor Level of Consciousness: reorient the client. Sedation can last for a few hours and affect cognition.
- Discharge: once the patient is awake and responsive with easy breathing and acceptable CP clearance, they may be discharged from the recovery room.
Continuing Care
Care for the postoperative client can continue in the ward. The primary concern is to promote optimal functioning, reducing pain, and wound care:
- Optimal Respiration: coughing, deep breathing, incision splinting, early ambulation, and turning in the bed are all potential exercises for maintaining and improving respiration by the patient.
- Optimal Circulation: early ambulation and leg exercises
- Optimal Nutrition
- Optimal Fluid and Electrolyte Balance: monitor IV, I&O, drains, dressings, and the return of peristalsis (flatus, bowel movement)
- Pain Control: analgesics and comfort measures
- Wound Care
Postoperative Discomforts
- Pain appears as the most prevalent postoperative discomfort once anesthesia begins to dissipate. The anesthesiologist handles pharmacologic pain management given initially via IV, moved to IM prn, then oral analgesia prn. The nurse offers diversional activities (television, etc.), avoids undue pressure to the operative side (client teaching about turning, splinting, coughing, etc.)
- Urinary Retention from anesthesia, anticholinergic drugs, and the use of urinary catheters. This predisposes the patient to UTI, marked by the presence of dysuria and fever.
- Paralytic Ileus, a temporary paralysis of the large intestine due to organ manipulation and anesthesia. The nurse identifies the presence or relief of paralytic ileus through the auscultation of bowel sounds. Diet is only resumed once bowel activity has resumed.
- Diet progression: NPO, clear liquid, general liquid, soft, then diet as tolerated or therapeutic diet (if prescribed)
- Hiccups can be a result of pathogenesis. This appears due to hyperventilation, increasing oxygen and decreasing carbon dioxide. This is corrected via re-breathing techniques, such as cupped hands or paper bags.
Postoperative Complications
- Hemorrhage: blood loss of more than 1,000 mL of blood. Cumulatively, this is determined by weighing used sponges, checking the suction bottle, pads, drains, etc. Hemorrhaging may occur from:
- Undue pressure on the operative site, especially during the transfer from the operative table to the stretcher, then from the stretcher to the patient bed.
- Improper ligation of blood vessels during surgery.
- Management: coagulants (Hemostan), pressure, monitoring (VS, I&O), possible blood transfusion
Arterial bleeding results in fast drops in blood pressure. Return to the operating room is required.
- Infection: the invasion of pathogenic microorganisms. This manifests as inflammation, redness, pain, and exudates.
- Factors affecting infection rate:
- Age (extremes of age)
- Nature of injury
- Duration of surgery
- Break in the sterile technique
- Improper wound dressing: start with the inside of the drain (if applicable), then the outside, then the wound.
- Management: antibiotics, antiinflammatory, analgesia, antipyretic, gram-staining/culture sensitivity (GSCS)
- Factors affecting infection rate:
- Urinary Tract Infection due to urinary retention; results in urinary frequency, dysuria, flank pain, and possible fever.
- Management: GSCS, antibiotic, analgesic, antipyretic
- Nursing Actions: increase oral intake, change catheters, monitor VS and I&O