This is the first note for CA1 ‘24 – ‘25 that will be centered around questions. These kinds of discussions are often non-linear and topics are bound to jump between systems or areas. This page will cover the most common drugs in the board exam, some disease processes, and some emergency and disaster nursing, etc.
This was presented as a set of eleven questions given on 11/24/2024 by Prof. Ferdinand Valdez RN, MAN, MPH of the Royal Pentagon Review Specialists, Inc.
Pharmacology
A COPD client prescribed Theophylline is having her serum drug levels checked as baseline to determine client compliance with her medication regimen. Which of the following baseline values would alert the nurse?
10 µg/ml
12 µg/ml
15 µg/ml
18 µg/ml
Answer
- 10 µg/ml
Theophylline, generic name Aminophylline, is a bronchodilator drug that is effective at a serum concentration of 10 to 19 mg/dL. The patient receiving their next dose is reminded to adhere to their medication regimen if the baseline level (trough levels) are found to be too low to adequately exert its therapeutic effect on the patient.
A client with a history of seizure disorder is admitted with seizure activity. A bolus of phenytoin is administered through IV and a serum phenytoin level is drawn. The nurse determines that the therapy has been most effective in which laboratory result?
3 µg/ml
8 µg/ml
16 µg/ml
24 µg/ml
Answer
- 16 µg/ml
Phenytoin, generic name Dilantin, is an anticonvulsant drug that is effective at a serum concentration of 10 to 19 mg/dL. Only option 3 shows a serum concentration that falls within this range.
A client who has been receiving digoxin therapy for heart failure began showing signs of toxicity. Which of the following laboratory values indicate the
Serum K+ of 3.2, Serum Digoxin Concentration of 1.6 µg/ml
Serum K+ of 3.5, Serum Digoxin Concentration of 1.8 µg/ml
Serum K+ of 3.3, Serum Digoxin Concentration of 1.9 µg/ml
Serum K+ of 3.4, Serum Digoxin Concentration of 2.0 µg/ml
Answer
- Serum K+ of 3.4, Serum Digoxin Concentration of 2.0 µg/ml
Digoxin (Lanoxin) is a cardiac glycoside (inotrope) that improves cardiac output by improving the contractility of the heart. It exerts its therapeutic effect in serum concentrations of 0.5 to 1.5 mEq/L and begins producing toxic effects at 2.0 mEq/L. Digoxin may cause hyperkalemia.
Magic Twos in Drug Monitoring
The Magic Twos is a table containing the most common drugs involved in the board exam. They follow the mnemonic D-LADA:
| Generic | Class | Therapeutic Window | Toxicity* | Indications |
|---|---|---|---|---|
| Digoxin (Lanoxin) | Cardiac Glycoside; Inotrope | 0.5–1.5 mEq/L | 2 | Congestive Heart Failure |
| Lithium (Eskalith) | Antimanic | 0.6–1.2 mEq/L | 2 | Bipolar Disorder |
| Aminophylline (Theophylline) | Bronchodilator | 10–19 mg/dL | 20 | COPD/CAL |
| Dilantin (Phenytoin) | Anticonvulsant | 10–19 mg/dL | 20 | Seizures |
| Acetaminophen (Tylenol) | Non-narcotic Analgesic | 10–30 mg/dL | 200 | Mild (1–3 pain scale) to Moderate Pain (4–6 pain scale) |
* need to add units
Arthritis
Acetaminophen is a part of pharmacologic management for those with osteoarthritis or rheumatoid arthritis. These are musculoskeletal disorders that produce joint pain and potential loss of function if unmanaged. Read also: Arthritis by Dr. Ferrer.
Osteoarthritis is common in obese and old patients, where the major weight-bearing joints (cervical spine, lumbar spine, knees) degenerate through wear-and-tear.
- Characteristic Pain Pattern: morning pain for less than 30 minutes. It is localized, asymmetrical, and non-systematic.
- Deformities: Heberden’s (distal metacarpal joint) and Bouchard’s (proximal metacarpal joint) nodes.
Rheumatoid Arthritis is a chronic, autoimmune, idiopathic disorder that affects the joints (and other systems).
- Characteristic Pain Pattern: stiffness that occurs for more than 30 minutes that appears systemically (all joints), symmetrically, and bilaterally
- Manifestations: Subcutaneous nodules, Raynaud’s phenomenon, and Swan-neck deformity of the fingers.
| OA | RA | |
|---|---|---|
| Descriptors/Key Words | Degenerative, Obesity, Old Age, Bone Spurs | Autoimmune, Idiopathic |
| Affected Joints | Weight-bearing Joints | Small Joints |
| Deformities | Heberden, Bouchard | Swan-neck |
| Pain Characteristics | Morning Stiffness, <30 minutes | Morning Stiffness, >30 minutes |
| Localized, Unilateral | Systematic, Bilateral | |
| Swimming as Relief | ✔️ | ✔️ |
| Medication | Injected Steroids | Oral Steroids |
Congestive Heart Failure
The major goal of therapy for a client with heart failure and pulmonary edema would be to:
Improve respiratory status
Increase cardiac output
Decrease peripheral edema
Enhance comfort
Answer
- Increase cardiac output
The disease process in heart failure is a decreased cardiac output. The main goal of therapy is to improve cardiac output by correcting the disease process. In pulmonary edema, the MAD DOG interventions are used: morphine, aminophylline, digitalis, diuretics, oxygen, and gases (ABGs).
Which of the following interventions are priorities during an exacerbation of left-sided heart failure? Select all that apply.
Metered Dose Inhaler of Albuterol
Tripod Position
Morphine
IV Fluids
Incentive Spirometer
Triamterene
Answer
2 (Tripod Position), 3 (Morphine), 6 (Triamterene)
The tripod position is used in orthopnea to improve lung expansion and oxygenation. Morphine is given for vasodilation, pain reduction, and as a sedative. Triamterene is a diuretic.
Congestive Heart Failure
The failure of the heart to pump blood towards systemic circulation. Cardiac output plummets and congestion (backing up of blood) occurs. The causes for CHF is outlined through the mnemonic FAILURE:
- Faulty Heart Valves: failure of the tricuspid valve results in right-sided heart failure (RSHF) and failure of the mitral valve results in left-sided heart failure (LSHF).
- Arrhythmias, specifically atrial fibrillation.
- Infarction, specifically myocardial infarction. Heart failure is among the most common complications of MI.
- Lineage: heredity
- Uncontrolled Hypertension
- Recreational Drug Use: cocaine, nicotine
- Evaders, also known as microorganisms, especially Group A Beta-Hemolytic Streptococcus (GABHS), a triggering microorganism for rheumatic fever/rheumatic heart disease/endocarditis that results in mitral valve stenosis.
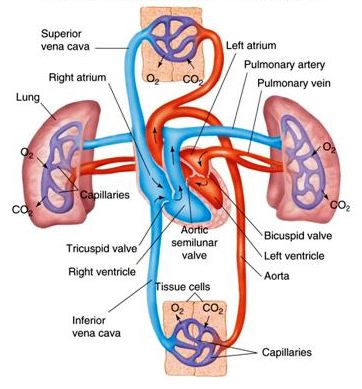
Adult Circulation
It is highly beneficial to have a solid foundation on adult circulation to understand the pathophysiology of left- and right-sided heart failure. Below is a diagram for a quick review: © McGraw-Hill
Left-Sided Heart Failure
- Pulmonary Edema/Congestion: the lungs feed into the left side of the heart. If it fails to pump, blood backs up into the lungs and becomes congested. This will result in fluid “leaking” out of the lungs, producing
- Pulmonary edema, pink-tinged frothy sputum.
- Difficulty of Breathing: dyspnea, orthopnea, paroxysmal nocturnal dyspnea.
- Adventitious breath sounds: rales, crackles, and wheezing.
- Anorexia and generalized body malaise.
- Lateral displacement of the apical pulse due to enlargement of the ventricles— cardiomegaly. The apical pulse, also known as the point of maximal impulse, is normally found between the 4th to 5th intercostal space along the left midclavicular line, just under the left nipple.
- Cyanosis from hypoxia
- S₃: an additional, abnormal heart sound called a ventricular gallop.
Right-Sided Heart Failure
The right side of the heart receives blood from the superior vena cava and inferior vena cava.
- Jugular Vein Distention
- Pitting edema: congestion increases fluid volume as blood pressure and cardiac output is inadequate, as an attempt to compensate. This, as well as the increasing hydrostatic pressure, allows fluid shifting from the intravascular space into interstitial spaces.
- Ascites: shifting of fluid into the peritoneal cavity.
- Weight Gain directly from fluid retention. 1 liter of fluid retained is equal to 1 lb. of weight gain.
- Hepatosplenomegaly: enlargement of the liver and spleen, which are both part of the portal venous system. Congestion cause them to enlarge from blood volume and edema.
- This also results in jaundice (skin, sclera) and pruritus/urticaria (due to bile salts).
- Esophageal Varices: distention of the esophageal veins, which are potential sources of upper GI bleeds.
- Anorexia and generalized body malaise.
Diagnostic Procedures
- Chest X-ray: visualization of cardiomegaly
- Echocardiography: ultrasound of the heart, revealing a distended, dilated heart. This also measures the ejection fraction:
- Ejection Fraction: the volume of blood in the heart ejected with each stroke, expressed in percentage. This is normally 55% to 70%. In heart failure, this goes down to <40%.
- Angiography: revealing the presence of a blocked artery, if such is the cause of the heart failure.
- Brain Natriuretic Peptide (BNP) B-type: a substance found in the blood in all cases where the ventricles become distended. In heart failure, this is produced by fluid volume overloading.
- Normal: ≤100
- Mild Elevation: 100–299
- Mild Heart Failure: ≥300
- Moderate Heart Failure: ≥600
- Severe Heart Failure: ≥900
Management
The mnemonic MAD DOG may be used for the interventions used in pulmonary edema (not sure about this yet; based on online sources).
- Morphine Sulfate: a narcotic/opioid analgesic used for pain, anxiety, and vasodilation. This drug can depress respirations and blood pressure, and as such prompts the nurse to assess blood pressure and respiratory rate prior to administering doses.
- Aminophylline (Theophylline): a bronchodilator to improve respiratory status. This is derived from sources similar to those used for caffeine— avoid caffeine (coffee, tea, chocolate, carbonated drinks) to prevent tachycardia, palpitations, restlessness, irritability, and agitation.
- Diuretics: drugs that enhance urinary elimination to reduce fluid volume. This is generally divided between potassium-wasting and potassium-sparing diuretics:
- Potassium-Wasting Diuretics: Bumex, Furosemide (Lasix), Hydrochlorothiazide, Mannitol. These affect the loop of Henle or the distal tubules (loop diuretics, thiazides)
- Furosemide (Lasix), oral or intravenous, takes effect in 5–10 minutes, with effects lasting up to 6 hours.
- These diuretics naturally produce hypokalemia.
- Potassium-Sparing Diuretics: Spironolactone (Aldactone), Amiloride, Triamterene
- These diuretics naturally produce hyperkalemia.
- Both types can produce hypovolemia, hypotension, and hyponatremia.
- Potassium-Wasting Diuretics: Bumex, Furosemide (Lasix), Hydrochlorothiazide, Mannitol. These affect the loop of Henle or the distal tubules (loop diuretics, thiazides)
- Digoxin (Lanoxin): a cardiac glycoside that exerts a positive inotropic effect and negative chronotropic effect. Check the patient’s pulse rate prior to administration— withhold the dose if bradycardia is observed.
- Digoxin also increases potassium levels. Potassium is normally 3.5–5.0 mEq/L.
- Monitor for signs of toxicity, because the therapeutic window of digoxin is very small. In order,
- Gastrointestinal manifestations: anorexia, nausea and vomiting, diarrhea
- Bradycardia
- Confusion
- Visual Disturbances: photophobia, xantopsia (yellow spots)/chloropsia (greenish vision/halos)
- Oxygen: high flow oxygen (4–6 L/min.)
- Gases: ABG analysis of O₂ and CO₂
- Oxygen: normally 80–100 PaO₂. Hypoxia occurs in respiratory dysfunction.
- Carbon Dioxide: normally 35–45 PaCO₂. Hypercapnia occurs in respiratory dysfunction.
Emergency Nursing
A male employee walks into the workplace clinic reporting that he was struck by lightning while working on his truck bed. He appears alert but reports feeling faint. Which assessment will the nurse perform first?
Open airway
Entry and exit wound
Pulse characteristics
Cervical spine injury
Answer
- Pulse characteristics
Lightning will act as a natural defibrillator. The patient, speaking, does not have an airway obstruction. A cervical spine injury is unlikely due to the patient’s alert and motor status (walks). Entry and exit wounds can occur with lightning, but the focus should be placed on a “feeling of faintness”.
A 58-year-old female client has superficial partial-thickness burns to the anterior head, face and neck; the entire left arm; the anterior of the right arm; the posterior trunk; the entire right leg; and the back of the left leg. Use the Rule of Nines to calculate the total body surface area that is burned.
63%
68%
72%
54%
Answer
- 63%
Body Part Full Burned Head 3% 1.5% Face 3% 1.5% Neck 3% 1.5% Left Arm 9% 9% Right Arm 9% 4.5% Thorax 18% 9% Abdomen 18% 9% Left Leg 18% 9% Right Leg 18% 18% Total: 63% Emergency medical technicians transport a 28-year-old ironworker to the emergency department. They report that the patient fell from a two-story building. The patient has a large contusion on the left chest, a hematoma in the left parietal area, a compound fracture of the left femur, and is in a coma. The patient is intubated and is being given manual resuscitation. He is maintaining an oxygen saturation of 92%. Which intervention by the nurse has the highest priority?
Assessing the left leg
Assessing the pupils
Placing the client in a Trendelenburg position
Assessing the level of consciousness
Answer
- Assessing the left leg
The patient has a compound fracture of the left femur. Being in close proximity to large blood vessels (femoral artery, femoral vein), this is a potentially major site of bleeding. Following the ABCs of life, airway and breathing has been established and is being maintained via intubation and Ambu-Bag. Circulation is the final step that is addressed only by Option 1.
Emergency Nursing
What is the collaborative goal of the nurse, physician, physical therapist, and nutritionist to patients with Parkinson’s?
To improve muscle endurance
To reduce ataxia
To build muscle strength
To maintain joint flexibility
Answer
- To maintain joint flexibility
One of the major manifestations of Parkinson’s is cogwheel rigidity. The goal is to maintain rather than to “improve” or “build” as the degenerative changes of Parkinson’s are irreversible. Ataxia is not a symptom of Parkinson’s.
Parkinson’s Disease
Parkinson’s Disease, also known as “shaking palsy”, “hypokinetic rigid syndrome”, and “paralysis agitans” is a degenerative disorder of the substantia nigra at the basal ganglia of the brain, which reduce dopamine production.
Dopamine is responsible for gross voluntary movement, relaxation, coordination, and mood/pleasure/attention reward.
Parkinson’s appears characteristically with:
- Pill-rolling Tremors, as one of the early signs of the disease.
- Tremors at rest, as one of the most common symptoms. This involves the hands, arms, legs, lips, mouth, and tongue.
- Bradykinesia is the slowness of movement. This manifests in voluntary movement such as in getting up from a chair.
- Cogwheel Rigidity is rigidity that appears as a jerky, racket-like resistance to passive movement.
- Stooped Posture: rigidity and postural instability produces a forward-flexed posture.
- Shuffling, Propulsive Gait: the center of gravity of a patient with Parkinson’s is shifted forward (postural instability), causing them to shuffle (small, quick steps forward; bradykinesia) and have difficulty stopping (festination). These are major risks for falls. Ensure safety.
- Fatigue
- Mask-like Facial Expression, appearing as a flat affect. Blinking is also decreased.
- Monotonous Speech
- Drooling due to a decreased ability to swallow and as part of autonomic changes and dysphagia (difficult swallowing).
- Autonomic Changes:
- Increased secretions: sweating, lacrimation, seborrhea (oily skin)
- Constipation as gastrointestinal motility decreases
- Decreased sexual capacity
- Mood Lability: dopamine is a happy hormone. Its deficiency along with the nature of the disease (irreversible, progressive) may lead to depression and increased suicide risk.
Miscellaneous
Which of the following categories would be appropriate for a nurse to include in a rehabilitation teaching plan of a patient who is a paraplegic?
Self-catheterization
Assisted coughing
Adapted feeding techniques
Compensatory swallowing
Answer
- Self-catheterization
A paraplegic is a patient whose lower half of the body is paralyzed. In contrast, monoplegia involves one limb, and quadriplegia involves all limbs below the level of the neck. A patient whose lower body is paralyzed will require knowledge on self-catheterization due to paralysis of the bladder. Assisted coughing, adapted feeding techniques, and compensatory swallowing are all activities involving the upper half of the body.
Which of the following foods should a client with leukemia avoid?
White Bread
Stewed Apples
Carrot Sticks
Medium Rare Steak
Answer
- Carrot Sticks
A patient with leukemia, a cancer of the blood, primarily affects white blood cells through abnormal proliferation of immature white blood cells (blasts). Such a patient will become immunocompromised (↓ neutrophils), alongside being anemic (↓ RBC) and prone to bleeding (↓ platelets). Raw vegetables and fruits, fresh produce, fresh flowers, and other sources of microorganisms are contraindicated. Reverse isolation is used. A medium rare steak is not raw meat.