Labor and Delivery is the expulsion of all the products of conception. Any parts retained will result in uterine atony, which enhances bleeding. The length of gestation is 9 months or 37 to 42 weeks.
- Contraction is prevented by progesterone which acts against estrogen, oxytocin (main hormone of contraction), fetal cortisol, and prostaglandin. Once progesterone fails to hold back the contractile stimulation, labor begins.
- Progesterone decreases on the ninth month because of the placental degradation after it reaches its lifespan limit. This starts contractions, and the mother enters labor and delivery.
More theories of labor include:
- Oxytocin Theory: the pressure of the fetal head on the cervix in late pregnancy stimulates the posterior pituitary gland to secrete oxytocin, which cases uterine contractions.
- Uterine Stretch Theory: the stretching of the uterus to an adequate size results in increased production of prostaglandin and oxytocin.
- Aging Placenta Theory: after maturation, more pressure is exerted on the fundal portion, the usual placental site, and the most contractile portion of the uterus. It is believed that the resultant diminished blood supply to the area causes contraction.
Labor begins with the premonitory signs of labor:
- Lightening: the entrance of the presenting part into the pelvic inlet, which relieves dyspnea and enhances urinary frequency. This occurs one to two weeks prior to delivery in primigravida, and one to two days prior to delivery in labor.
- Weight Loss: secondary to nesting behavior of around 2 to 3 pounds prior to labor and delivery
- Increased Tension and Fatigue: tension from beginning contractions (Braxton Hicks) and fatigue from nesting behavior.
- Cervical Changes: effacement (thinning of the internal os; to 100%) and dilatation (widening of the diameter of the external os; 0 to 10 cm).
- In primigravida, dilatation then effacement occurs. In multigravida, simultaneous dilatation and effacement, or effacement before dilatation occurs.
- “Nesting Behavior”: last minute preparation for delivery; purchasing maternal and child goods
- Rupture of the Bag of Water
- Braxton Hicks: painless, irregular contractions that are signs of false labor.
| Parameter | False Labor | True Labor |
|---|---|---|
| Origin of Pain | Abdomen | Lower back (lumbosacral) to the abdomen; Girdle pain |
| Effect of Walking | Pain is relieved | Pain intensifies |
| Uterine Contractions | Non-progressive | Progressive; frequency and duration increases, interval decreases. Intensity and pain increases. |
| Bloody Show | (-) | (+); a sudden discharge of blood. |
| Cervical Changes | (-) | (+); effacement and dilatation. Dilatation is the most important criteria for true labor. |
| Bag of Water | (+) | (-); ruptured. If intact during true labor, a prolonged labor may occur. The occurrence of a rupture is overt, which is why this is the most commonly asked question to pregnant clients to determine true labor. |
| Effect of Sedation on Contractions | Effective | Ineffective |
Bag of Water
The infant must be delivered within four hours of rupture as this permits the occurrence of ascending infection. Once likely, the mother’s temperature is checked to detect the onset of fever.
The color of the water is normally clear. If stained (green or yellow) with meconium, the fetus may be in distress. Check for the fetus’ heart rate (normally 120 to 160). In early distress, the finding is tachycardia, which progresses to bradycardia.
If the bag of water does not rupture, which prolongs labor, an amniotomy (intentional rupture) is performed to increase uterine contractions to hasten the first stage of labor (Dilatation)
Stages of Labor (DEPR)
- Dilatation (from the onset of true labor to full dilatation)
- Nursing Responsibility: monitor the progress of labor, determining the progression of labor through the three phases of this stage.
| Parameter | Latent | Active | Transitional | |
|---|---|---|---|---|
| Dilatation | 0 – 3 cm | 4 – 7 cm | 8 – 10 cm | |
| Duration | <40s | 40 – 60s | 60 – 90s | |
| Frequency | q5min | q3 – 5min (2–3 UC/10 min.) | q1 ½ – 2min | |
| Intensity | Mild | Moderate | Strong (but not hypertonic) | |
| Maternal Behavior | Cooperative | Ambivalent/Less Cooperative | Uncooperative |
- Expulsion (from full dilatation to the delivery of the baby)
- Nursing Responsibility: delivery the baby safely
- Placenta (from the delivery of the baby to the delivery of the placenta)
- Recovery (two hours after placental expulsion)
Five Ps of Labor and Delivery
The five Ps of labor are all necessary in order to undergo a normal pregnancy. With problems in any of the five Ps will result in difficult labor and delivery: dystocia.
- Power: the forces that will push the baby out. The primary source of power is contraction that originates from the myometrium of the fundus in the upper uterus. The secondary source of power is the ability of the mother to bear down or push.
- Maternal pushing is not done without full effacement and dilatation, as this may result in laceration of the cervical canal. An uncontrollable urge to push is felt during the transitional phase of labor, but should be held back through panting (“blowing candle” technique, alleviates urges; relaxes the abdomen).
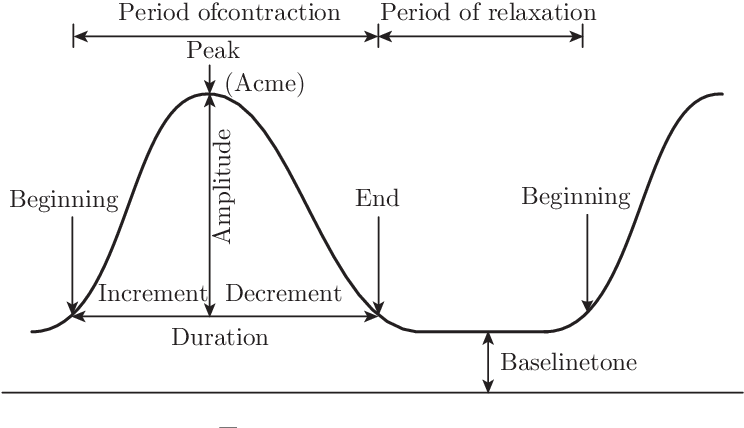
Parameters of Uterine Contractions
- Frequency: the time from the onset of one contraction to the onset of the next contraction (“Increment to Increment”)
- Duration: the length of one contraction (“Increment to Decrement”)
- Interval: the time from the end of one contraction to the start of the next contraction (“Decrement to Increment”)
- Passageway: the birth canal and its structures (pelvis, cervical canal, vaginal canal). The cervical canal is tasked with effacement and dilatation, while the vaginal canal requires adequate distensibility.
- Type of the Pelvis: gynecoid and anthropoid are those fitted to pregnancy
| Cavity | AP | Transverse | Oblique |
|---|---|---|---|
| Inlet | 11 | 13 | 12 |
| Cavity | 12 | 12 | 12 |
| Outlet | 13 | 11 | 12 |
- Passenger: (see prev. discussion on this):
- The size of the baby affects the ease or difficulty of delivery, especially with cephalopelvic disproportion when the fetus is too large to pass through the pelvis. The normal birth weight of a neonate is 2,500 to 3,400 (maximum of 4,000) grams.
- Number of children: normally one; if more, then the issue of positioning becomes a problem, especially if one baby is transverse while the other baby is longitudinal.
- The positioning of the passenger affects the ease of delivery.
- Fetal Presentation: cephalic (face, brow, vertex, occiput), breech, transverse
- Attitudes: flexion (normal) or extension of the head
- Lie: longitudinal (cephalic, breech), transverse, oblique
- Position: most commonly LOA, landmarks: occiput, mentum, sacrum
Auscultation of Fetal Heart Tone
The fetal heart tone is best heard along the back; for cephalic babies (occiput, mentum), the lower quadrant is used, while the upper quadrant is used for breech babies (sacrum). The same side of the abdomen is used for the occiput and sacrum, while the opposite side of the abdomen is used for the sacrum.
- Psyche: the maternal state of mind and psychological safety. This may be supported physically, emotionally, and psychologically through prenatal checkups, companion of choice, or through the nurse (therapeutic touch, updating the mother on the progress of labor)
- Placental Factors: dysfunctions of the placement or detachment of the placenta, among other abnormalities:
- Placenta Previa: the placement of the placenta in the lower uterus, ranging being lateral to the passageway or completely obstructing the passageway.
- Abruptio Placenta: the early detachment of the placenta from the uterus.
Exercise
Mrs. Troy is at term and undergoing labor. She started to feel contractions at 9:55 AM that ended at 9:56:10 AM. This was followed by another contraction at 9:57:40 AM that ended at 9:58:55 AM. Her cervix is 8 cm dilated with a ruptured bag of water. The baby is at +2 station. Examination reveals a vertex presentation with the back at the right side of her abdomen. She had 1 abortion and a stillbirth at 35 weeks. She left home her twin sons born at 40 weeks. Determine her GPTPALM, stage, phase, presentation, attitude, lie, position, and FHR auscultation site. Calculate the duration, frequency, and interval of the (first) contraction.
Answers
- G4P221121: four pregnancies, two deliveries (twins, stillbirth), two term babies, one preterm baby, one abortion, two living children, and one multiple delivery.
- The pregnancy is in Stage 1 (Dilatation), Phase 3 (Transitional)
- The baby has a cephalic presentation with an attitude of flexion, lying longitudinally, positioned ROA, with the FHR auscultation site at the right lower quadrant.
- The first contraction lasted for 70 seconds. The interval to the next contraction took 1 minute and 30 seconds. The frequency is 2 minutes and 40 seconds.
Essential Intrapartal and Newborn Care (EINC)
A mandated series of steps in the care of the newborn during and immediately after delivery. The ENC (December 2009) attempted to answer the Millennium Development Goals 4 and 5 (Maternal and Child Mortality, respectively). The goal is to decrease mortality rates by 40%. This was achieved for mothers, but only 20% for neonates. To push neonatal health further, the previously established ENC was updated to the EINC (May 2012) to further improve outcomes of pregnancy.
In Pre-Pregnant and Childbearing-Age Women
- Healthy Lifestyle: exercise and the avoidance of alcohol (Low IQ; cognitive impairment) and smoking (Vasoconstriction; SGA, IUGR). Even residues of these can affect a pregnancy even after cessation.
- Health Teachings:
- Prevention of venereal diseases (STDs), family planning, and conception.
- Nutritional requirements: (inc.)
| Component | Amount |
|---|---|
| Calories | 2,000/day |
| Iron | 30 mg/day |
| Salt | Iodized, not Rock Salt |
In Pregnant Women
Exercises and avoidance of smoking and alcohol are still practiced during pregnancy.
- Prenatal checkups are utilized to track the progress of gestation. The minimum recommended is four visits (DOH), at least once per trimester, and one at the final month of pregnancy.
- Dieting requirements:
| Component | Amount |
|---|---|
| Calories | 2,300 to 2,500/day |
| Iron | 60 mg/day |
| Folic Acid | 400 mcg/day |
| Calcium | 1,200 mg/day |
| Protein | 60 mg/day |
| Vitamin A | 10,000 IU 2nd Trimester |
| Elemental Iodine | 250 mg (1 cap)/pregnancy; can relieve need for iodized salt |
| Increased fiber and fluid | Prevent constipation |
- Exercises:
- Walking (best)
- Pelvic Rocking: the assumption of a squatting position, and rocking the pelvis forward and backwards. This relieves back pain.
- Tailor Sitting: The assumption of indian seating on a non-slip mat, and stretching of the perineal tissues. This makes the perineum supple (elastic, stretchy) to prevent easy laceration.
- Squatting: with support from a sturdy surface; this strengthens perineal muscles.
- Kegel’s Exercise: strengthens the perineal (pelvic floor) muscles.
- Antenatal Steroids: the administration of steroids for pregnant women with (a) history of premature birth, (b) risk of preterm birth (hypertension, diabetes mellitus, anemia), (c) history of vaginal bleeding during pregnancy, and (d) actual preterm labor. These steroids are given from the 24th to 28th week to promote surfactant production (fetal lung maturity).
- Dexamethasone: 6 mg IM every 12 hours for four doses.
- Betamethasone (Celestone): 12 mg IM every 24 hours for two doses. In emergent cases, this is used because of its higher dosage.
For patients with history of premature labor, risk of premature labor, or history of bleeding, the patient can complete the dosage. Otherwise, in actual premature labor, one dose is enough.
In the Labor Room
- Admit the patient when they reach the active phase (4 cm dilatation or 2-3 contractions every 10 minutes), with her companion of choice (COC) to provide continuous maternal support.
- Positioning: any upright position (sitting, fowlers, standing, squatting, walking), as long as the bag of water has not ruptured, whichever the patient deems more comfortable. This utilizes gravity to promote cervical effacement and dilatation. Once ruptured, the woman is placed on a left lateral (side-lying) position.
- End of NPO Status: the woman can continue consuming food and fluids. This provides the energy for maternal pushing. Eating can be done until about half of the active phase; 6 cm, with easy-to-digest foods.
- End of IV Infusion, including oxytocin incorporation. IV fluids were also used to provide glucose, but with the continuation of eating and drinking, these are discontinued. Oxytocic drugs also produce the risk for atony.
- Perform IE to monitor the progress of labor. This is done less than five times to reduce the risk of infection. The standard for frequency is every four hours, at most every two hours.
- Empty the bladder. A distended bladder may obstruct fetal descent; an empty bladder promotes fetal descent.
- No more shaving: there was no significant difference between unshaved and shaved women during labor.
- No more enema, due to its tendency to increase blood pressure.
- Partography is used in order to monitor the progress of labor.
In the Delivery Room
Prior to the transfer to the delivery room, prepare the environment.
- Set the temperature (25°C to 28°C).
- Eliminate air drafts.
- The AC unit is closed just before the baby is delivered to avoid hypothermia.
Safe Delivery Techniques
- Maintain the semi-upright position, with the COC present (continue providing maternal support). This position utilizes gravity (again) to aid in delivery, and make bearing down easier as the natural motion is to draw the chin to the chest.
- Perform Ritgen’s Maneuver to support the perineum during crowning, preventing lacerations.
- Check for cord coil once the head and neck are exposed. If present, the cord is clamped and cut.
- Oxytocin IM is given one minute after the baby is out (after initiation of early skin-to-skin contact).
- Perform the four newborn protocols.
Procedures Not Routinely or Not Performed
- Amniotomy: only performed when indicated, primarily in prolonged labor and delivery, decided by the doctor.
- Episiotomy: only performed when indicated, when the head is deemed likely to cause laceration of the perineum as decided by the doctor.
- Coached pushing: not done to avoid the valsalva maneuver. However, pushing is not allowed if cervical effacement and dilatation have not been completed.
- Fundal pushing can produce lacerations.
- Brandt-Andrew’s Maneuver: not used; rather, controlled cord traction with counter traction is used to express the placenta.
- Cord Milking, which may result in neonatal circulatory overload.
- Methergine IM
Chronological Arrangement of EINC Deliveries
- Gloves: 2 pairs, both worn at the same time to first deliver the baby, then to clamp and cut the cord.
- Towels: 2 pieces, one on the lower abdomen of the mother for catching and drying the baby. The second towel is used to wrap the back of the baby (ensure skin-to-skin contact)
- Pat the baby dry, rather than rubbing. This maintains the vernix caseosa, which is a thermoregulatory and bacteriostatic medium.
- Bonnet: 1 piece, placed on the head of the baby to maintain heat after drying.
- Oxytocin IM in syringe ready for injection to the mother. This is given one minute after the baby is out, coinciding with the end time of drying and early skin-to-skin contact.
- The WHO promotes the use of two precautions prior to administration of oxytocin: check for uterine contraction and the possible presence of a second baby.
- Oxytocin can increase blood pressure. It must be less than 140/90 for administration. Notify the physician if this threshold is crossed.
- Cord dressing materials: cord clamp, kelly, bandage scissors.
- Remove the last worn pair of gloves used for delivering the baby.
- Clamping and cutting is done after pulsations have stopped, at a maximum of three minutes.
- The cord clamp is placed first, 2 cm from the base of the umbilicus, then the kelly clamp 5 cm from the base (3 cm from the cord clamp). It is cut 1 cm from the cord clamp, in between the two clamps.
- Once cut, the umbilicus is air-dried. It dries and falls off by itself in 7 to 10 days.
Evolution of Cord Care
- Previously, daily cord care was done with 70% alcohol b.i.d. to enhance drying of the umbilical cord. However, this method kept the cord moist with the 30% water the remains after alcohol evaporates, which promotes infection.
- Then, betadine 10% was used. However, this caused skin irritation and scratching by the newborn.
- After the ENC arrived, room-temperature pre-boiled water was used to clean the umbilical cord. However, this retained the original issue of retention of moisture of the cord, which promoted infection.
- In EINC, nothing is applied to the cord to let it dry by itself.
- Empty kidney basin used for disposable items such as needles and syringes.
- Kidney basin with 5% chlorine solution to disinfect the scissors and kelly used during cord dressing.
- It is after this period that the placenta is delivered in AMTSL (Active Management of the Third Stage of Labor). This period starts immediately after oxytocin is administered.
- The CCTCT (controlled cord traction with counter traction) technique is used for delivering the placenta. Again, the Brandt-Andrew’s Maneuver is no longer done, as this may continue to irritate lacerations if present. In CCTCT, (a) press down on the lower abdomen (counter-traction), then (b) pull on the cord with a straight line of force.
- After expulsion, the completeness of the placenta is checked. The normal 15 to 20 cotyledons are found on the maternal side of the placenta. The perineal area of the mother is quickly cleaned.
- Empty space; time for breastfeeding. This period lasts for the first 90 minutes after delivery, following the last step of the four newborn protocols.
- Signs of the readiness for feeding: (1) mouth-opening (sucking reflex), (2) kicking, and (3) grasping. With these signs, the mother is instructed to bring the child to her chest, and let the baby find the nipple for feeding.
- To do so, the baby’s head is placed between the breasts and the baby’s head is turned towards the areola and nipple. The head of the baby may turn with the rooting reflex that functions to locate and find the nipple. This reflex is incited by touching the corner of the mouth, after which the head turns towards the side of the corner stimulatd.
- Despite the baby’s blurry and limited vision (~9 inches), the baby is able to see the nipple and grasps (grasping reflex) the nipple, which the newborn brings to its mouth.
- Signs of the readiness for feeding: (1) mouth-opening (sucking reflex), (2) kicking, and (3) grasping. With these signs, the mother is instructed to bring the child to her chest, and let the baby find the nipple for feeding.
- Eye prophylaxis with erythromycin (ophthalmic ointment) is done after successful breastfeeding. This is applied from the inner canthus to the outer canthus. It is done to prevent blindness from sexually-transmissible diseases the child may obtain after traversing the birth canal. This condition is known as ophthalmia neonatorum.
- Vitamin K: an anticoagulant applied to the vastus lateralis to make up for the lack of normal flora (E. Coli) in the intestinal environment, which is contributory in the synthesis of Vitamin K. The normal flora develops naturally with contact with the mother.
- Hepatitis B Vaccine: 0.5 mL IM at the vastus lateralis to protect against hepatitis B. If screening shows the presence of HBV in mothers, then Hepatitis B immunoglobulin is also used.
- BCG Vaccine: 0.05 mL ID on the upper right deltoid.
A tuberculin syringe is used (1-mL, 5/8" needle with 26-25 gauge) for Vit. K, HBV, and BCG administration
- Stethoscope for assessment
- Tape measure for anthropometric measurement:
| Measurement | Normal Range |
|---|---|
| Head Circumference (above the brow) | 33 to 35 cm |
| Chest Circumference (nipple line) | 31 to 33 cm |
| Abdominal Circumference (above the umbilicus) | 31 to 33 cm |
| Birth Length (cephalocaudal) | 47 to 54 cm |
| Birth Weight | 2,500 to 3,400 (max of 4,000) grams |
Newborn Protocols (Principles of Unang Yakap)
- Immediate Drying of the newborn within 30 seconds. This prevents hypothermia with the poor thermoregulation of the baby.
- Skin-to-skin Contact within the next 30 seconds (1 minute total) to promote bonding, promote heat regulation, and promote transfer of skin flora (protects against infection, particularly streptococcal and staphylococcal infection). This prevents hypoglycemia (energy stores are used to keep the baby warm) and infection.
- Properly Timed (Delayed) Cord Clamping and Cutting within three minutes (until cord pulsations stop). This prevents anemia of the baby (allow more blood to enter fetal circulation before pulsations stop). Do not milk the cord, as this may result in circulatory overload, which can delay the closure of the foramen ovale.
- Rooming-in and Early Initiation of Breastfeeding (for the first 90 minutes): the mother and newborn is kept in the same room to promote the initiation of breastfeeding and bonding.
Partography
A partograph includes three components: progress of labor, fetal parameters, and maternal parameters. Its use is indicated once the woman enters the active phase of labor (4 cm CD, 2-3 UC/10 min)
Composite Partograph
(I didn’t document this part as much)
- Fetal Parameters (top section): fetal heart rate
- Progress of Labor (middle section): plot with the alert and action line. This is a visual representation of the dilation of the cervix and the station of the head.
Regardless of Gravidity, the cervix should dilate at least one centimeter per hour in a normal pregnancy.
- Maternal Parameters (lower section)
Guidelines for Use
- In the plot, one time column is subdivided into two columns: the left border of the left column is used for plotting dilatation (intersecting the line with an X). For any other parameter on the column, they are written centered.
- The cervical dilation found during the first internal examination is placed along the alert line. This means that the starting column with tracking is the column that contains the point at which the alert line represents the actual cervical dilatation; for example, start three columns from the left if the initial cervical dilatation was found to be 6.
- The time plotted after the first
Timedesignation is at an interval of one hour each (actual hour on clock). The row aboveTime,Hours, is a sequence of hours passed since she entered active labor; starts with 1 upon admission, and so on. If this exceeds eight hours while the mother remains in the active phase, the patient becomes a candidate for emergency cesarean section. Amniotic Fluidcontains notation of the following:C- clear,I- intact,M- meconium-stained,B- bloody,A- absent (ruptured)Moulding: graded with0: open suture,+: closed suture,++: one plate rises,+++: two plates overlapContractions: a measurement of frequency every 10 minutes. This contains a maximum of five contractions per minute. If contracts are more frequent, report to the obstetrician. The number of cells is filled from the bottom of the column, chronologically, according to the occurrence of contractions. This uses a visual representation of contraction quality:- Dotted: <20 seconds
- Line-shaded: 20-40 seconds
- Fully shaded: >40 seconds
- The IV section (outdated), simply writes medications and fluids given.
- Pulse and BP: a margin drawn for the systolic and diastolic pressure, with the pulse marked with a dot along the same column.
Simplified Partograph
Vaginal Bleeding:0- no bleeding,+- mild bleeding,++- moderate bleeding, and+++- strong bleedingAmniotic Fluid: same as the notation for the composite partograph.- The beginning of the plotted column must coincide with the alert line, same as before.
Nursing Responsibilities in the Alert Area
- Notify the doctor. The doctor writes a referral letter for the facility the patient will be transferred to. The nurse aids in the preparation of the letter.
- Contact CEmONC (Comprehensive Emergency Obstetric Newborn Care) Facility, a blood-banking facility with an operating room that may handle a possible cesarean section.
- Prepare Emergency Transport Service: ambulance, barangay patrol, etc.
- NPO for food, but not fluid; drinking is still allowed. This is to prepare for a cesarean section.
- Bladder emptying
- Continue monitoring both the mother and child.
One CEmONC facility caters to 500,000 population, while a BEmONC (basic) facility caters to 125,000 population.