Reference
Salustiano, R. (2024). High-Risk Pregnancy. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 117–195). C&E Publishing, Inc.
A high-risk pregnancy is one in which the mother or fetus has a significantly increased harm, damage, injury, or disability, and loss of life or death. It often requires specialized care from specially trained healthcare providers in specialized facilities.
Factors Contributing to Maternal and Neonatal Deaths (DOH)
The majority of maternal deaths directly result from pregnancy complications occurring during labor, delivery, and the post-partum period. These include:
- Hypertension
- Post-partum Hemorrhage
- Severe infections
- Other medical problems arising from poor birth spacing, maternal malnutrition, unsafe abortion, the presence of concurrent infections (TB, Malaria, STIs), and lifestyle diseases like hypertension and diabetes.
The majority of neonatal deaths within the first week of life are due to asphyxia, prematurity, severe infections, congenital anomalies, newborn tetanus, among other causes.
The DOH specifies three DELAYs that increase maternal and neonatal mortality:
- Delay in identification of complications
- Delay in referral
- Delay in the management of complications
RISKs that contribute to maternal and neonatal deaths:
- Mistimed, unplanned, unwanted, and unsupported pregnancies
- Not securing adequate care during the course of pregnancy
- Delivering without being attended to by skilled health professionals (e.g. midwives, nurses, and doctors) and lack of access to emergency obstetrics and newborn services (EmONC)
- Not securing proper postpartum and newborn care for the mother and her newborn, respectively
Risk Factors in Pregnancy
- Demographic Factors: three main parameters relevant to pregnancy are:
- Age: being less than 16 or over 35 years old
- Weight: being underweight (less than 90 lbs) or overweight (more than 150 lbs) poses a risk for SGA/LGA infants respectively.
- Height: being less than five feet is a risk for cephalopelvic disproportion
- Socioeconomic Status:
- Inadequate finances
- Overcrowding, inadequate housing, poor hygiene
- Nutritional deprivation
- Severe social problems
- Unplanned, unprepared pregnancy, especially among adolescents. This is rooted in poverty and poor education.
- Obstetric History:
- History of infertility or multiple gestations
- Grandmultiparity (>5G)
- History of abortion, ectopic pregnancy
- Previous losses: fetal death, stillbirth, neonatal death, perinatal death
- Previous operative birth: cesarean section, midforceps delivery
- Previous uterine or cervical abnormality
- Previous abnormal labor: prematurity, postmaturity, prolonged
- Previous high-risk infant: LBW, LGA/macrosomia, neurologic deficits, birth injury, malformation
- Previous hydatidiform mole
- Current OB Status
- Late or no prenatal care
- Maternal anemia
- Rh sensitization
- Antepartal bleeding: placenta previa and abruptio placenta
- Pregnancy-induced hypertension
- Multiple gestation
- Premature or postmature labor
- Polyhydramnios
- Premature rupture of membranes (PROM)
- Fetus inappropriately large or small; abnormality in tests for fetal well-being; abnormality in presentation
- Maternal Medical History/Status
- Cardiac or pulmonary disease
- Metabolic disease: diabetes, thyroid disease
- Endocrine disorders: pituitary, adrenal
- Chronic renal disease: repeated UTI, bacteriurea
- Chronic hypertension
- Venereal and other infectious diseases
- Major congenital anomalies of the reproductive tract
- Hemoglobinopathies
- Seizure disorder
- Malignancy
- Major emotional disorders and mental retardation
- Maternal Habits/Habituation (SAD habits)
- Smoking during pregnancy
- Regular alcohol intake
- Drug use/abuse
Diagnostics in High-Risk Pregnancy and Prenatal Determination of Fetal Status
Ultrasonography
An ultrasound is a non-invasive diagnostic procedure utilizing high-frequency sound waves to detect intrabody structures. It is advantageous in that it is accessible, does not ionizing radiation, and excellently depicts female genital anatomy. It is the imaging of choice in the initial evaluation of gynecologic emergencies. It may be used to:
- Confirm pregnancy in early gestation.
- Obtain fetal parameters: viability, growth, number, position, presentation, structural abnormalities, heart tones, and age of gestation via biparietal diameter of the fetal head (most accurate from 12 to 24 weeks, 9.5 cm in a mature fetus)
- Detect placental location or abnormality, such as placenta previa and H-mole.
- Assist in other procedures, such as amniocentesis.
Procedure
- Drink 1 quart of water 2 hours before the procedure.
- Do not void prior to the procedure.
- Prepare transmission gel to be spread over the abdomen.
- Provide psychological support to both mother and father. Explain the reason, risks, benefits, and preparations required for the procedure. Explain that no known risk to the mother and fetus is associated with infrequent exposure to high-frequency sound waves.
- Encourage verbalization of fears and concerns. Explain that the procedure is noninvasive, safe, requires no confinement, has no need for dye or contrast, and takes a short period (about 30 minutes) to accomplish.
Nonstress Test (NST)
A non-stress test observes fetal heart tones (FHT) in relation to fetal movements as a test of fetal well-being. In a normal fetus, FHT increases with fetal movements. The following findings may be observed:
- Normal; Reactive Nonstress Test: the FHT accelerates greater than 15 BPM above baseline, lasting 15 or more seconds in a 10 to 20 minute period with fetal movement. If found in a high-risk client, the pregnancy may continue.
- Abnormal; Nonreactive Nonstress Test: FHR does not accelerate with fetal movement. If found in a high-risk client, further testing is performed, such as a Biophysical Profile.
Procedure
The mother is positioned semi-Fowler’s or left lateral position slightly turned to the left.
- Check her blood pressure
- Explain the procedure: its duration is 30 to 60 minutes, and requires no hospitalization; this can be done on an ambulatory basis. The mother will need to activate the “mark button” for each fetal movement felt.
- Prepare external electronic FHT monitor with an ultrasound transducer and tocodynamometer to trace fetal activity and/or uterine activity.
Oxytocin Challenge Test (OCT)/Contraction Stress Test (CST)
Contractions are induced to observe the response of the fetus as a test of feto-placental well-being. A normal finding must show three contractions within 10 minutes each showing no late decelerations. Late decelerations are decelerations in FHT even after the peak of contraction, and lasts even after the contraction has ended. This indicates that the fetus is not receiving a proper amount of oxygen.
Procedure
The mother is positioned semi-Fowler’s or left lateral position.
- Check her blood pressure 15 minutes before and prior to the exam.
- Explain the procedure: its duration is 1 to 3 hours. The mother receives oxytocin in an increasing dosage until three contractions is observed in 10 minutes. This may be done on an outpatient basis.
- This also requires an external electronic FHT monitor with an ultrasound transducer and tocodynamometer to detect uterine activity.
Nipple Stimulation Contraction Test
The breasts are stimulated with the rolling of nipples or warm towel application. This stimulates the posterior pituitary gland to secrete oxytocin, contracting the uterine musculature (and breast tubules)./ In this test, the fetal response to uterine contractions is tested. The monitoring and interpretations are the same as in the oxytocin contraction test.
Biophysical Profile
A scoring system that utilizes ultrasound assessments to determine the presence of chronic asphyxia. A score of 10 to 8 is normal (low risk), 4 to 6 is suspected for chronic asphyxia, and a score of 0 to 2 is a high risk for chronic asphyxia.
| Biophysical Variable | Normal (2) | Abnormal (0) |
|---|---|---|
| Fetal Breathing Movements | Grater than or equal to one episode of 30 seconds or more of fetal breathing movement in 30 minutes | Absence of 30 seconds or longer of fetal breathing movement in 30 minutes |
| Gross Fetal Movement | Three or more discreet movements of the body or any limb in 30 minutes | Two or fewer discreet movements of the body or a limb in 30 minutes |
| Fetal Tone | One or more episodes of extensions and flexion of the fetal limb(s) or trunk Opening and closing of the hand is considered normal | Either slow extension with return to partial flexion, movement of the limb in full extension, or absent fetal movement |
| Reactive Fetal Heart Rate | Two or more episodes of accelerations for 15 BPM or more lasting for 15 seconds or longer in 20 minutes; associated with fetal movement | Less than two episodes of acceleration of the fetal heart rate or acceleration of less than 15 BPM in 20 minutes |
| Qualitative Amniotic Fluid Volume | One pocker or more of fluid measuring 1 cm or more in two peripendicular planes | Either no pockets or a pocket of 1 cm or less in two perpendicular planes |
Amniocentesis
The amniotic sac is entered to aspirate amniotic fluid for a variety of diagnostic exams to determine fetal well-being. In a fetus at 15 to 18 weeks of gestation, up to 30 mL of amniotic fluid is aspirated. Many methods for analysis can be done for a variety of indications:
- Foam Stability Test/Shake Test: the most common test to determine fetal lung maturity, finding the L/S ratio to be 2:1 in mature lungs.
- Age of Gestation (AOG) can be found with creatinine levels (2.0 mg in 36 weeks, more onwards) or a nile blue stain (staining lipid cells)— 20% of aspirated cells should stain orange, indicating a fetal weight of at least 2,500 grams.
- Alpha-Fetoprotein (AFP): can be measured which, if elevated, can indicate the presence of a neural defect (spina bifida, tracheoesophageal atresia).
- Genetic disorders and sex-linked disorders can be checked with chromosomal studies and sex chromosome determination.
- Rh Incompatibility results in high levels of bilirubin (from isoimmunization). The mother is evaluated for intrauterine transfusion or delivery.
- Inborn errors of metabolism can be determined through biochemical analysis of fetal cell enzymes.
- Fetal distress may be determined with the presence of meconium while in cephalic presentation (not significant when breech).
Procedure
- Secure informed consent. Inform the mother of the major risks of the procedure: trauma to the fetus, placenta, umbilical cord, and maternal surface; infection; abortion; preterm labor.
- Prepare for ultrasonography to locate the placenta and provide visualization during a blind procedure.
- Void prior to the procedure in order to prevent injuring the distended bladder with a needle. Similar to a normal ultrasound, the mother drinks 1 quart of water 2 hours before the procedure.
- Prepare equipment: g 20–22 3” to 6” needle and local anesthesia for the abdomen.
- Provide psychological support: inform the patient of the details of the procedure: up to 30 mL of amniotic fluid is aspirated at 15 to 18 weeks of gestation.
- Aftercare: monitor the client for 30 to 60 minutes. Observe for side effects such as vaginal discharge, increasing uterine/fetal activity, and fever or chills.
Others
- X-ray, specifically lateral pelvimetry, is used for the determination of pelvic size and shape, indicated for those with suspected cephalopelvic disproportion, a history of injury or disease of the pelvis and spine, previous difficult deliveries, and cases of maternal deformities or limps.
- Special Estriol Determination is a measurement of feto-placental well-being by analyzing serum or 24-hour urine (more common) samples for estriol.
- Normally, estriol rises by 12 to 50 mg/day at term.
- Abnormally, a sudden drop in estriol (more than half of previous levels) indicate fetal distress. Persistence of this low level means fetal well-being is compromised.
- Chorionic Villi Sampling (CVS) is the earliest test done to test fetal cells. This is done via a catheter passed through the cervix.
- Percutaneous Umbilical Blood Sampling (PUBS) is used in the second and third trimesters, aspirating and testing cord blood. Ultrasound is used to locate the umbilical cord.
Complications of Pregnancy
Pregnancy-Induced Hypertension (PIH)
A disorder characterized by proteinuria, edema, and hypertension appearing after the 20th to 24th week of pregnancy and disappearing 6 weeks after delivery. This occurs in 7% to 10% of all pregnancies and is one of the major causes of maternal and neonatal mortality. Its actual cause is unknown.
- Etiologic Factors:
- Nulliparity with extremes of age (<18, >35)
- Severe nutritional deficiency: low protein and low calorie diet
- Coexisting conditions: diabetes mellitus, multiple pregnancies, polyhydramnios, chronic hypertension, renal disease
- Assessment Findings: symptoms resulting from generalized vasospasm and arteriolar vasoconstriction increasing peripheral resistance, decreased tissue perfusion, and hypertension. The decreased tissue perfusion affects the kidneys, brain, and uterus in particular.
- Kidneys: ischemia causes glomerular lesions and membrane damage, resulting in disturbed functions. This results in proteinuria, hypoproteinemia, altered a/g ratio, altered blood osmolarity, and fluid shifting (intravascular → interstitial).
- The kidneys also release angiotensin in response to decreased perfusion, resulting in further vasospasm and hypertension.
- Brain: cerebral arteriospasm and edema cause cerebral hypoxia and CNS irritability manifested in (a) visual disturbances— double vision, blurring, dimness of vision, (b) hyperreflexia/hyperirritability, (c) convulsion, and (d) coma in severe cases.
- Uterus: decreased placental perfusion results in an SGA baby, and precipitates abruptio placenta.
- Kidneys: ischemia causes glomerular lesions and membrane damage, resulting in disturbed functions. This results in proteinuria, hypoproteinemia, altered a/g ratio, altered blood osmolarity, and fluid shifting (intravascular → interstitial).
- Signs and Types of Preeclampsia
| Signs | Mild Preeclampsia | Severe Preeclampsia |
|---|---|---|
| Hypertension | 140/90 or systolic increase of 30 mm Hg or more above the baseline; diastolic rise greater than 15 mm Hg or more. | 160/110 or systolic increase at or above 160 or more than 50 mm Hg over the baseline; diastolic rise greater than 110 mm Hg or more on two readings taken 6 hours apart after bed rest. |
| Proteinuria | 1+ or 1 g/day | 3+ to 4+ or 5 g/day or more |
| Edema | Weekly weight gain of >1 lb. per week | Excessive weight gain of 5 lbs. per week or more. - Epigastric pain (edema of the liver capsule) - Cerebral edema: headache, vision changes, hyperreflexia, dizziness, vomiting, disorientation. |
| Oliguria | Absent; 500 mL or more in 24 hours | Present; 400 mL or less in 24 hours |
| IUGR | Absent | Present |
| Others | Hypoproteinuria, hemoconcentration, hypernatremia |
Eclampsia
Eclampsia is associated with convulsions and coma. Severe headaches and epigastric pain may mean an oncoming convulsion. The first nursing action if the patient complains of a severe headache or epigastric pain is to check blood pressure. The first objective sign of a convulsion is rolling of the eyeballs.
- Nursing Planning and Intervention
- Prevention: Health Teaching
- Well-balanced dieting with high protein (increase blood osmolarity, prevent fluid shifting)
- Supplemental iron: 30 to 60 mg per day in the second and third trimester, continued 2 to 3 months postpartum
- Increased caloric intake by 10% in pregnancy (total 2,300 – 2,500 kcal/day)
- Sodium is not restricted as it may decrease circulating volume, cause fluid and electrolyte imbalance, and eliminate vital nutrients.
- Adequate rest and sleep in the left lateral (Sims’) position.
- Regular prenatal care with careful monitoring for danger signs: (a) visual disturbances, (b) severe, persistent headache and dizziness, (c) digital and periorbital edema, (d) irritability, and epigastric pain.
- Well-balanced dieting with high protein (increase blood osmolarity, prevent fluid shifting)
- Treatment and Nursing Care
- Maintain bedrest in the left lateral recumbent position: increase tissue perfusion, induce diuresis, reduce supine hypotensive syndrome
- Provide a high-protein diet with moderate sodium: replace protein losses (from proteinuria), retain fluid in the intravascular compartment, and reduce edema.
- Frequent monitoring: the room should be easily accessible from the nurse’s station:
- Vital signs
- Intake and output: oliguria is a grave sign; diuresis is good.
- Daily weight/edema: degree and distribution of fluid retention; periorbital edema is a dangerous sign found in severe preeclampsia.
- Reflexes: particularly of deep tendon reflexes in magnesium sulfate toxicity.
- Onset and progress of labor, and signs of placental abruption.
- Administering drugs as ordered:
- Magnesium sulfate is used as an anticonvulsant.
- Prior to administration, check the respiratory rate. MgSO₄ can reduce respiratory rate by impeding the respiratory center and the smooth muscles of respiration.
- Check the knee-jerk reflex to determine toxicity before administering next doses. It should at least be 1+.
- Check blood pressure.
- Keep 10% calcium gluconate, the antidote for MgSO₄, ready.
- Procaine hydrochloride may be mixed with MgSO₄ to reduce irritation and pain; this requires a doctor’s order. The same is true for lidocaine/lignocaine (Xylocaine). In 2023 BEmONC standards, the standard procedure is to add 1 mL of 2% lignocaine in the same syringe with 5 grams of 50% MgSO₄ for deep IM in each buttock (dose is divided to reduce irritation). Use the Z-track technique and do not massage the site.
- After administration, monitor BP, RR, DTRs, I&O, and FHT.
- Hydralazine (Apresoline; 5 mg IV over 1 to 2 minutes) is used as an antihypertensive. Give with meals and monitor blood pressure. This is done for patients with ≥160 mm Hg/≥110 mm Hg. Other antihypertensives include:
- Nifedipine immediate-release only: 5–10 mg p.o. q30min until desired blood pressure is achieved, max. of 30 mg
- Labetalol oral: 200 mg p.o. q1° until desired blood pressure is achieved, max. of 1,200 mg in 24 hours
- Labetalol IV: 10 mg IV, double dose every 10 minutes to 80 mg until goal is achieved, max. of 300 mg, then switched to oral. Not used in congestive heart failure, asthma, or hypovolemic shock.
- Diazepam (Valium) as an anxiolytic, promoting rest and is used as an adjunct in seizure disorder. Blood pressure is monitored while lying and standing (orthostatic hypotension), assess degree of anxiety, give with food or milk for GI symptoms, and give sugarless gum and frequent sips of water for dry mouth.
- Magnesium sulfate is used as an anticonvulsant.
- Prevent convulsions: reduce environmental stimuli (dim, quiet room, restrict visitors), and utilize a room close to the nurse’s station. Magnesium sulfate may be administered as ordered. Emergency items (airway, cath. set, IV fluids, emergency drugs) are prepared. Monitor closely for signs of impending convulsion:
- Severe (frontal) headache
- Severe epigastric pain
- Sharp cry
- Fixed, unresponsive eyes
- Facial twitchings
- Hyperreflexia
- Provide care during convulsions: first priority— maintain a patent airway by positioning the patient on a lateral position, gentle suctioning, and provide oxygen as ordered; second priority— promote safety and prevent injury by setting bedrails, and not using restraints. Read: Magnesium Sulfate Therapy
- Record and monitor the type of convulsion: duration, progress, resultant coma, or bowel or bladder evacuation.
- Continue strict monitoring for 48 hours after delivery because convulsions may still occur in the postpartum period.
- Prevention: Health Teaching
Abortion
Abortion is the termination of pregnancy before the age of viability (20 to 24 weeks). In general, the death of a fetus before 28 weeks of pregnancy is referred to as a miscarriage (WHO, 2023d). In general, abortions may be spontaneous or induced.
A spontaneous abortion occurs without medical or mechanical intervention. Its most common cause is a defective ovum/congenital defect, followed by unknown causes. Other causes include maternal viral infection, malnutrition, trauma, congenital defects of the reproductive tract, incompetent cervix (most common in habitual abortion), hormonal imbalance (decreased progesterone), increased temperature (fever), systemic diseases (DM, thyroid dysfunction, severe anemia), environmental hazards, and Rh incompatibility.
- Prevention focuses mainly on lifestyle factors: healthy dieting, exercise, avoidance of smoking, alcohol, and drugs, limiting caffeine, controlling stress, and maintaining a healthy weight.
- An abortion may present with signs of vaginal bleeding or spotting, uterine/abdominal cramps, passage of tissues or products of conception, and signs related to blood loss/shock (pallor, tachycardia, tachypnea, cool clammy skin, restlessness, oliguria, air hunger, and hypotension).
An induced abortion may be:
- Elective or voluntary in regions where it is permitted (abortions are among the most common medical procedure in the U.S.)
- Therapeutic for medical reasons or in cases of rape or incest, or in cases where the fetus is determined to have significant anatomical, metabolic, or mental deformity
- Medical with the use of medications (Mifegymiso is widely available in Canada) to induce abortion at home, potentially preferrable over surgical methods
- Criminal if the the abortion is done outside of a legitimate medical facility, often resulting in maternal morbidity or mortality. This is a felony for those to assist, advise, or perform the abortion, and ruled as a homicide if the mother who had undergone an abortion dies as a result of the procedure.
Philippines' Abortion Provisions (Center for Reproductive Rights)
- Constitution of the Republic of the Philippines (1987), Article II, Section 12: The State recognizes the sanctity of family life and shall protect and strengthen the family as a basic autonomous social institution. It shall equally protect the life of the mother and the life of the unborn from conception. The natural and primary right and duty of parents in the rearing of the youth for civic efficiency and the development of moral character shall receive the support of the Government.
- Revised Penal Code of the Philippines, Act. No. 3816 of December 8, 1930, Articles 256–259; Section 2: Infanticide and Abortion
- Article 256: Intentional Abortion— any person who shall intentionally cause an abortion shall suffer (a) reclusion temporal if violence is used, (b) prision mayor if without violence yet without consent of the woman, and (c) prision correccional in its medium and maximum periods if the woman shall have consented.
- Article 257: Unintentional Abortion— the penalty of prision correccional in its minimum and medium period shall be imposed upon any person who shall cause an abortion by violence, but unintentionaly.
- Article 258: Abortion practiced by the woman herself or by her parents— the penalty of prision correccional in its medium and maximum periods shall be imposed upon a woman who shall practice abortion upon any person who shall practice abortion upon herself or shall consent that any other person should do so. This is also imposed upon the parents of the pregnant woman or either of them. Any woman who shall commit this offense to conceal her dishonor, shall suffer the penalty of prision correccional in its minimum and medium periods.
- Article 259: Abortion practiced by a physician or midwife and dispensing of abortives— the penalties of Art. 256 shall be imposed in the maximum period upon any physician or midwife who, taking advantage of their competency, shall cause an abortion. Any pharmacist who, without proper prescription from a physician, shall dispense any abortive shall suffer arresto mayor and a fine not exceeding 1,000 pesos.
| Spontaneous Abortions | Bleeding | Abdominal Cramps | Cervical Dilatation | Tissue Passage | Fever |
|---|---|---|---|---|---|
| Threatened | Slight | May or may not be present | None | None | No |
| Inevitable | Moderate | Moderate | Open | None | No |
| Complete | Small to negative | Moderate | Close or partially open | Complete placenta with fetus | No |
| Incomplete | Severe (bleeds the most) | Severe | Open with tissue in cervix | Fetal or incomplete placental tissue | No |
| Missed | None to severe incoagulopathy | None; No FHT with UTZ | None | None | No |
| Septic | Mild to severe | Severe | Close or open with or without tissue | Possible; foul discharge | Yes |
Habitual Abortion
Three or more consecutive abortions can be considered habitual. This is most commonly caused by an incompetent cervix, and occurs as any of the types of spontaneous abortions mentioned above. This is often detected in the threatened phase, and cervical closure via the McDonald (temporary) or Shirodkar-Barter (permanent) cerclage may be employed.
Treatment and Management
- Medical Termination: the use of medical means to terminate the pregnancy.
- Early pregnancy: antiprogestin (mifepristone), antimetabolite (methotrexate), prostaglandin (misoprostol) can cause abortion by increasing uterine contractility.
- Second-trimester abortion: the use of a single, high-dose intravenous oxytocin and prostaglandin administration, including prostaglandin E1 (misoprostol) pills and prostaglandin E2 suppositories.
- Surgery:
- Vacuum aspirator
- The use of a Laminaria tent to enhance dilatation. This is a ripening, hygroscopic dilator/osmotic dilator that draws water from surrounding tissues and expands to gradually dilate the endocervical canal.
- Sharp dilation and curettage is not recommended due to greater blood loss, pain, and procedural time.
- Antibiotics: prompt intravenous broad-spectrum antimicrobials are instituted to prevent sepsis.
- Blood, plasma, and fluid replacement
- Blood tests: blood typing, Rh factor, Coombs test, serum fibrinogen, clotting time, platelet
- Habitual abortion: determine etiology, treatment of underlying cause, cerclage operation/cervical closure for an incompetent cervix.
- McDonald cerclage: temporary stitching done between 16 and 18 weeks, with the stitch removed around week 37 or at the time of labor.
- Shirodkar-Barter cerclage: permanent suturing done in the wall of the cervix. Future pregnancies will require cesarean section.
- Abdomen cerclage: the cervix is stitched shut at the very top of the cervical opening. This is only done when other methods are not viable. It is also permanent and evasive.
| Type | Nursing Care/Management |
|---|---|
| Threatened Abortion | - Advise complete bedrest for 24 to 48 hours. - Teach to save all blood clots passed and perineal pads used. - Advise prompt reporting to the hospital if bleeding persists or increases. - Prevention of abortion: avoid coitus or orgasm, especially around the normal time of menstrual period. |
| Inevitable Abortion | - Save or monitor clots, pads, or tissues for a correct diagnosis. - Monitor VS, blood loss, I&O, changes in status, and signs of infection, and refer any deviation. - Institute measures to treat shock as necessary: replace blood, plasma, and fluids as ordered. - Prepare for surgery. - Provide psychological support: non-judgmental attitude, encourage verbalization, reduce anxiety, and allow the patient to cry. - Prevent isoimmunization: administer RhoGAM as ordered if: the mother is Rh negative; the abortus is Rh positive, and Coombs test result is negative. |
Ectopic Pregnancy
An ectopic pregnancy is a condition where pregnancy develops outside of the uterine cavity: extrauterine pregnancy in which the blastocyst implants anywhere other than the endometrial lining of the uterine cavity. Nearly 95% of ectopic pregnancies implant in the fallopian tube most commonly as a mechanism of abnormal fallopian tube anatomy that alters normal embryo transport. The following are predisposing factors for an ectopic pregnancy:
- Fallopian tube narrowing or constriction, prior tubal pregnancy, prior tubal surgeries for fertility restoration, for ectopic pregnancy, or for sterilization, surgery of the fallopian tubes, and congenital anomalies of the fallopian tubes
- Pelvic inflammatory disease originating from Neisseria gonorrhea or Chlamydia trachomatis (salpingitis, endometriosis)
- Puerperal and postpartal sepsis
- Adhesions, spasms, and tumors
- IUD usage: the intrauterine device prevents pregnancy by preventing normal implantation
- Age: increasing maternal age raises the risk for ectopic pregnancy with those older than 40 carrying the highest risk. This has been attributed to age-related hormonal changes that alter tubal function.
Ectopic pregnancies can be classified according to location of abnormal implantation:
- Tubal: found in 90% to 95% of cases. Due to its thinness, tubal rupture occurs before 12 weeks. These have a high maternal morbidity and mortality when ruptured.
- Cervical
- Abdominal
- Ovarian
Assessment Findings and Diagnosis
- Amenorrhea or abnormal menstrual period/spotting— the most common sign
- Early signs of pregnancy: signs of tubal rupture
- Sudden, acute low abdominal pain radiating to the shoulder— Kehr’s sign (referred shoulder pain) or neck pain
- Nausea and vomiting
- Bluish navel (Cullen’s Sign) because of blood in the peritoneal cavity
- Rectal pressure because of blood in the cul-de-sac
- Positive pregnancy test in many women (50%)
- Sharp, localized pain when the cervix is touched
- Signs of shock/circulatory collapse
- Laboratory findings: low hemoglobin, low hematocrit, low hCG (normally 400,000 IU/24 hours), and elevated WBCs.
Diagnosis starts with clinical signs. Ectopic pregnancy is considered in any reproductive-aged woman with pain, uterine bleeding, and/or anemia.
- Ultrasonography is the study of choice for ectopic pregnancy. Two methods may be used:
- Transabdominal ultrasound (traditional)
- Endovaginal ultrasound: more diagnostic, but more invasive.
- Serial testing for hCG beta-subunit; serum β-hCG measurement offers a 100% accurate result.
- β-hCG monitoring with an ultrasound is the current standard for diagnosing an ectopic pregnancy.
- A laparoscopy may be used for direct visualization, but it is not commonly used.
- Hemogram: an additional fast and effective initial screen.
Treatment
Once diagnosed, ectopic pregnancies can be managed surgically, medically, or expectantly. Because of the potential for life-threatening bleeding, careful patient selection is essential.
- Surgical removal of the ruptured tube: Salpingectomy
- Management of profound shock: blood replacement when a rupture results to severe bleeding
- Medical management in unruptured ectopic pregnancy: methotrexate (MTX) is used to induce separation of the abortus. Distention of the tubes, separation pain, and hematoma formation may cause expected a common side effect of abdominal pain managed by analgesics. However, MTX is contraindicated in:
- Ruptured tubes
- Intrauterine pregnancy
- Immunodeficiency
- Breastfeeding
- Peptic ulcer
- Hepatic, renal, or hematologic dysfunction
Complications of an Ectopic Pregnancy
- Hemorrhage
- Infection
- Rh Sensitization: RhoGAM prevents isoimmunization and is given to an Rh-negative mother with an Rh-positive ectopic pregnancy with a negative Coombs test.
Nursing Management
- Carry out an on-going assessment for shock as one of the major complications of ectopic pregnancy. If present, implement shock treatment promptly:
- Position on a modified Trendelenburg
- Infuse D5LR solution for plasma administration, blood transfusion, or drug administration.
- Monitor VS, bleeding, and I&O.
- Provide Physical and psychological support: both pre-operative and post-operative
- Anticipate grief and possible guilt responses.
- Anticipate fear related to potential disturbances in childbearing capacity in the future.
Hydatidiform Mole
An H-mole is a benign neoplasm of the chorion. The chorion fails to develop into a full-term placenta and instead degenerates into fluid-filled vesicles. This is common in the Orient and in people of low socioeconomic status, but its actual cause is unknown. Other risk factors include:
- Advanced or early maternal age
- Low socioeconomic status; low protein diet
- History of abortion and Clomiphene/Clomid therapy
Prognosis, Complications
80% of patients experience remission after D&C of the H-mole. However, the chorion may become cancerous; a choriocarcinoma. This is the most dreaded complication. Other complications includes:
- Hemorrhage: most serious during the early treatment phase
- Uterine perforation
- Infection
Assessment Findings and Diagnosis
- Brownish or reddish, intermittent, or profuse vaginal bleeding by 12 weeks.
- Spontaneous expulsion of molar cyst usually occurs between the 16th and 18th weeks of pregnancy; passage of a cyst.
- Rapid uterine enlargement; upon assessment, the fundus is found higher than expected based on the age of gestation.
- Symptoms of PIH appear before 20 weeks.
- Excessive nausea and vomiting due to highly elevated levels of hCG (1 to 2 million IU/24 hours). This high level of hCG also results in a positive pregnancy test.
- NO FETAL SIGNS— heart tones, parts, movements
- Abdominal pain
- Diagnostic Criteria:
- Passage of vesicles: the first sign that aids diagnosis.
- H-Mole Triad: (a) big uterus, (b) vaginal bleeding, intermittent, brownish, (c) hCG greater than 1,000,000 IU/L/24 hours.
- Ultrasound: no visible fetal sac; no fetal parts.
- Flat plate (KUB) of the abdomen after 15 weeks also shows no fetal skeleton.
Treatment
- Evacuation by D&C or hysterectomy if no spontaneous evacuation occurs.
- Hysterectomy if over 45 years old and no future pregnancy is desired, or if hCG levels remain increased even after D&C.
- hCG titer monitoring after evacuation for one year. In this period, no pregnancies should be had because early signs of pregnancy can mask the signs of a choriocarcinoma.
- Medical replacement of blood, fluid, plasma in the event of bleeding
- Chemotherapy for malignancy: Methotrexate is the drug of choice.
- Chest X-ray is used to detect early lung metastasis.
Nursing Management
- Advise bedrest
- Monitor VS, blood loss, molar/tissue passage, and I&O
- Maintain fluid and electrolyte balance, plasma, and blood volume through replacement as ordered.
- Prepare for D&C, hysterotomy, or hysterectomy as indicated.
- Provide psychosocial support: anticipate fear related to the potential development of cancer, and disturbance in self-esteem for carrying an abnormal pregnancy.
- Prepare for discharge: emphasize the need for follow-up hCG titer determination for one year, and reinforce instruction on no pregnancy for one year. Provide instructions for contraception if needed.
Incompetent Cervix
A condition characterized by a mechanical defect in the cervix causing cervical effacement, dilation, and expulsion of the products of conception in the mid-trimester of pregnancy. Pregnant women are at risk for an incompetent cervix if they (a) have a congenital defect of the cervix (short), (b) trauma to the cervix as in forceful dilatation, curettage, and difficult delivery, and (c) cervical lacerations procedures (conization, cauterization).
This appears as:
- Painless contractions resulting in the delivery of a dead or non-viable fetus
- History of abortions (habitual abortion)
- Finding of a relaxed cervical os on pelvic examination
Treatment and Nursing Management
- Cervical cerclage during the 14th and 16th week of gestation or prior to the next surgery. A suture or ribbon is placed beneath the cervical mucosa to close the cervix during pregnancy to help prevent pregnancy loss or premature birth. This may be done via:
- Shirodkar-Barter Cerclage: a permanent suturing of the cervix, with future pregnancies delivered via cesarean section.
- McDonald Cerclage: a temporary purse-string suturing of the cervix removed at term in preparation for a vaginal delivery.
- Nursing Implementation:
- Psychological support: low self-esteem; fear related to inability to complete pregnancy; and guilt or anticipatory grief related to loss of an expected baby.
- Post-cerclage procedure care:
- Bedrest: left-side lying position for a few days. Limit activity within 2 weeks of treatment.
- Maintain hydration, void regularly to keep the bladder empty.
- Perineal hygiene: wear a sanitary pad if necessary; change frequently.
- Showers or tub baths are permitted, but no douches or tampons should be used.
- Report danger sign: fever, chills, general aches, saturating one pad in less than 3–4 hours, foul-smelling or thick yellow discharge. An increasing clear, vaginal discharge and light spotting up to 3 days is normal.
- Continue maternal and fetal growth monitoring. Maintain routine prenatal care.
- Assess for signs of labor, infection, or premature rupture of membranes.
- Instruct the patient to promptly report and signs of labor.
- In labor, prepare stitch removal sets if McDonald cerclage has been performed.
Placenta Previa
The premature separation of an abnormally low implanted placenta. This is the most common cause of bleeding in the third trimester, occurring in 1:150 to 1:200 pregnancies. Risk factors for placenta previa include:
- Multiparity: the single most important factor
- Upper uterine segment dysfunction: decreased vascularity, scarring, tumors
- Advanced maternal age: >35 years
- Multiple pregnancy
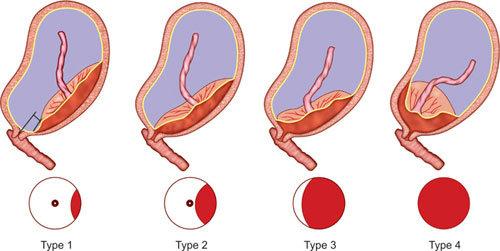
| Type | Description | Position |
|---|---|---|
| I | Low-lying | Placenta at the lower third of the uterus, but does not cover the internal os. |
| II | Marginal: may be considered low-lying | Placenta lies over the margins of the internal os. |
| III | Incomplete/Partial | Placental partly covers the internal os; within 2 cm of the internal os. |
| IV | Complete or Total | Placenta totally covers the internal os. |
Vaginal Delivery with a Previa
When the placental tip measures between 1 and 12 cm from the internal cervical os, up to 90% of these patients will deliver successfully via the vaginal route. As long as the inferior margin of the placenta is at least 2 cm from the internal os, there is no significant increased risk of bleeding during labor.
Assessment Findings and Diagnosis
- Painless vaginal bleeding of bright red, fresh blood in the third trimester (7th month). This may be slight or profuse coming after an activity, coitus, or internal examination.
- Soft, flaccid uterus with intermittent hardening if in labor
- Intermittent pain if placenta previa occurs secondary to uterine contractions in labor.
The determination of placenta previa is imaging through ultrasonography, giving a 95% accurate result and detects the site of the placenta.
Complications
- Hemorrhage
- Prematurity
- Obstruction of the birth canal
Treatment
- Watchful waiting, i.e., expectant management is prepared. Conservative management is used if the mother is not in labor, bleeding is not severe, and the fetus is still premature, stable, and not in distress.
- Amniotomy, an artificial rupture of the bag of water done to cause the fetal head to descent, compressing the site of bleeding to reduce bleeding.
- Double setup, the preparation of both vaginal and cesarean section delivery sets as contingency in suspected placenta previa. This is used for fetuses who are stable and at term whose mother is progressing well in labor. If the woman is not in labor or in shock, and/or the fetus is distressed, only the emergency classical cesarean section setup needs to be prepared.
- Vaginal Delivery may be used if the birth canal is not obstructed. Cesarean section is indicated if the lower uterine segment is occupied by the placenta.
After classical cesarean section,
Future pregnancies will also be terminated via cesarean section as the scar of a classical cesarean section is a major risk for uterine rupture, and is therefore a contraindication for vaginal delivery.
Nursing Management
- Maintain bedrest: left lateral recumbent with a head pillow.
- Do not perform an IE or vaginal examination, which may exacerbate bleeding and disrupt or detach the placenta.
- Careful assessment: vital signs, bleeding, onset and progress of labor, fetal heart tone
- Prepare for diagnostic ultrasonography
- Institute shock measures if necessary. Bleeding is rarely life-threatening but may become profuse with internal examination.
- Provide psychological and physical comfort
- Prepare for conservative management, double setup, or classical CS.
- Observe for bleeding after delivery because the lower uterine segment is less contractile than the upper uterine segment.
Abruptio Placenta
An abruptio placenta is a complication of late pregnancy or labor characterized by premature partial or complete separation of a normally implanted placenta; also termed as accidental hemorrhage and ablatio placenta. This is the second leading cause of bleeding in the third trimester; occurring in 1:300 pregnancies second only to placenta previa. Risk factors for abruptio placenta include:
- Maternal hypertension; PIH, renal disease
- Sudden uterine decompression such as in polyhydramnios and multiple gestation.
- Advanced age
- Multiparity
- Short umbilical cord
- Trauma; fibrin defects
| Types | Description |
|---|---|
| Type I | Classic concealed, covert, central type. The placenta separates at the center, causing blood to accumulate behind the placenta, hiding the presence of bleeding. External bleeding does not appear to match the severity of shock. |
| Type II | Marginal, overt, external bleeding type. The placenta separates at the margins, allowing old blood (dark red, brown) to spill out. In this type, external bleeding matches the severity of shock. |
| Type III | Mixed. Some part of the blood remains concealed, while some are expelled. |
Assessment Findings and Diagnosis
- Painful vaginal bleeding in the third trimester.
- Rigid, board-like, and painful abdomen.
- Enlarged uterus from concealed bleeding; signs of shock that may be disproportional to external bleeding.
- Tetanic contractions if in labor— alternating contraction and relaxation does not occur.
Diagnosis is based on clinical signs and symptoms and an ultrasound to image retroplacental bleeding.
| Areas of Major Differences | Placenta Previa | Abruptio Placenta |
|---|---|---|
| Placental Location | Lower uterus | Upper uterus |
| Bleeding | Painless, vaginal, fresh, bright red | Painful, often concealed, dark, old blood if external |
| Abdomen | Soft/flaccid; during labor with intermittent hardening and softening corresponding with uterine contractions. | Hard, board-like; during labor, No characteristic intermittent hardening and softening of the abdomen. |
| Major Complications | Hemorrhage Prematurity Obstruction of the birth canal | Hemorrhage Couvelaire Uterus Disseminated Intravascular Coagulation (DIC) |
| PIH as a risk factor | PIH is not a risk factor | PIH is a major risk factor |
Complications
- Hemorrhagic Shock
- Couvelaire Uterus: blood enters the myometrium, preventing contraction.
- Disseminated Intravascular Coagulation (DIC) which can cause CVA, hypofibrinogenemia
- Renal Failure
- Infection
- Prematurity, Fetal Distress/Demise (IUFD) due to insufficiency from placental separation.
Clotting studies reveal the presence of DIC and clotting defects. The thromboplastin from the retroplacental clot enters maternal circulation and consumes maternal free fibrinogen, resulting in DIC and hypofibrinogenmia.
Nursing Implementation
- Maintain bedrest, LLR
- Careful monitoring: VS, FHT, Labor onset and progress, I&O (oliguria, anuria), uterine pain, and bleeding.
- Administer IV fluid, plasma, or blood as ordered
- Prepare for diagnostic examination; equipment and client teaching
- Provide psychological support: prepare for all examinations, explain steps of the procedure during the examination, and explain the results.
- Prepare for emergency birth via vagina or CS.
- Observe for problems after delivery:
- Couvelaire uterus that prevents contraction after delivery, which may result in postpartal hemorrhage
- Disseminated Intravascular Coagulation that results in hemorrhage (hypofibrinogenemia) and potential CVA (clotting)
- Prematurity, neonatal distress, neonatal morbidity, neonatal mortality
Hydramnios
Disorders of amniotic fluid volume, either excessive (hydramnios or polyhydramnios) or diminished (oligohydramnios)
- Normal: amniotic fluid at term (36 weeks) weighs up to 1000 mL, decreasing to only 100–200 mL or less post-term.
- Polyhydramnios: increased amniotic fluid volume greater than the upper limit of normal of 1,500–2,000 mL; arbitrarily, more than 2 L of amniotic fluid.
- Oligohydramnios: diminished amniotic fluid less than 500 mL; oligohydramnios means “scant amniotic fluid” and is diagnosed when an ultrasound reveals an amniotic fluid index (AFI) of 5 cm or less (normal AFI is 5–25 cm).
This occurs in about 1% of pregnancies. Acute hydramnios often appears earlier in pregnancy (16–20 weeks), and as a rule leads to labor before 28 weeks, or the symptoms become so severe that intervention become mandatory.
Risk Factors/Causes
- Fetal Anomalies: esophageal atresia is a common cause of hydramnios when the fetus is unable to swallow amniotic fluid.
- Fetal infection
- Anencephaly and spina bifida can also increase fluid volume when meningeal transudation increases.
- Excessive fetal urination, such as in gestational diabetes causing fetal hyperglycemia, resulting in osmotic diuresis.
Assessment Findings and Diagnosis
- Major symptoms are attributable to pressure exerted by the overdistended uterus: dyspnea, edema (abdominal wall, vulva, lower extremities), and oliguria (rarely; ureteral obstruction).
- Mirror syndrome: the maternal condition mirrors hydrops fetalis; develops edema and mild proteinuria.
Diagnosis begins with clinical findings: uterine enlargement, difficulty palpating fetal parts and difficulty hearing FHTs, and is confirmed via fetal ultrasound to image the fetus and amniotic sac.
Complications/Pregnancy Outcomes
- Common fetal malformations and chromosomal abnormalities
- Perinatal mortality
- Preterm delivery
- Most common maternal outcomes: Abruptio placenta, uterine dysfunction, postpartum hemorrhage
- Abnormal fetal presentation, umbilical cord prolapse
- (Oligohydramnios) Cord compression and increased risk for cesarean delivery.
Treatment and Nursing Management
Mild and moderate hydramnios rarely requires treatment.
- Hospitalization is indicated when dyspnea, abdominal pain, or difficulty ambulating are present.
- Amniocentesis can relieve maternal distress.
- Amniotomy may be used, but is disadvantageous as it is a risk for cord prolapse and abruptio placenta.
- Indomethacin Therapy: impairs lung liquid production, enhances absorption, decreases fetal urine production, and increases fluid movement across fetal membranes.
- Management of Oligohydramnios in late pregnancy depends on clinical situation. Evaluation for fetal anomalies and growth with close fetal surveillance is done due to the risk for abnormality, and delivery is recommended for fetal and maternal indications.
Nursing Management
The nurse promotes bedrest and comfort, aiding in dyspnea (semi-Fowler’s, high-Fowler’s) and assisting (if necessary) in repositioning every 2 hours.
Pre- and Co-existing Diseases of Pregnancy
Diabetes Mellitus
Diabetes mellitus is a chronic metabolic disorder characterized by a deficiency in insulin production by the islets of Langerhans (Type 1), altered insulin secretion and utilization (Type 2), or the effect of the metabolic changes in pregnancy on insulin production and utilization (Type 3) resulting in improper metabolic interactions of carbohydrates, fats, proteins, and insulin. This may be a concurrent disease in pregnancy or may have its first onset in pregnancy.
Risk Factors for Diabetes
- Family history
- Rapid hormonal changes in pregnancy
- Tumor/infection of the pancreas
- Poor diet/obesity
- Stress
- Inactivity/sedentary lifestyle
| Types | Name | Cause |
|---|---|---|
| Type 1 | Insulin-dependent Diabetes Mellitus | The exact cause is unknown— thought to be an autoimmune reaction destroying insulin-producing beta cells in the pancreas. Triggering factors include genetic and environmental factors (viral infection): - Human enteroviruses (HEV) has the strongest body of evidence for triggering T1DM. Sudden, early onset and development diagnosed in children, teens, and young adults. Insulin is a required treatment for survival. |
| Type 2 | Adult-Onset; Non-insulin-dependent Diabetes Mellitus | The cause for T2DM is also not exactly known. The body’s sensitivity and/or utilization of insulin become impaired, failing to keep blood sugar within normal levels. Gradual onset with slow development over many years diagnosed in adults. Treatment may be through diet and oral hypoglycemic agents or insulin. Prevention of T2DM can be achieved by maintaining healthy lifestyle changes: health food, losing weight, avoiding obesity, activity/regular exercise. |
| Type 3 | Gestational Diabetes Mellitus | The pancreas cease to produce enough effective insulin for the body due to normal metabolic and hormonal changes in pregnancy. Increased insulin antagonistic hormones produced by the placenta (primarily hPL) prevents the body from using insulin effectively, and hyperglycemia develops. |
Normal Metabolic Changes in Pregnancy
- Insulin-antagonistic hormones increase: cortisol, estrogen, progesterone, hPL raise maternal resistance to insulin, resulting in insulin’s ineffectiveness in using glucose at the cellular level.
- Increased metabolic rate in pregnancy causes an increased number of islets of Langerhans resulting in increased insulin production, which is rendered ineffective by the insulin antagonists (primarily hPL).
- If the pancreas cannot produce more insulin to reduce glucose levels, glucose crosses the placental barrier and, by resembling the growth factor, causes an extra-large fetus— macrosomia/LGA.
- Increased anterior pituitary gland activity; decreased tolerance for sugar.
- Elevated basal metabolic rate (BMR) and decreased carbon dioxide combining power, producing a tendency of metabolic acidosis.
- Normal lowered renal threshold for sugar and increased glomerular filtration rate produces glucosuria.
- Vomiting during pregnancy decreases carbohydrate intake and causes metabolic acidosis.
- Muscular activity in labor depletes maternal glucose, including glycogen stores, and requires increased carbohydrate intake.
- Hypoglycemia is common in the puerperium as involution and lactation occur.
- In existing diabetes mellitus, pregnancy makes blood sugar maintenance more difficult, and the potential for insulin shock and ketoacidosis (from discomfort, nausea, vomiting) are common.
- In the first trimester, insulin needs are stable. No increase may be necessary.
- In the second trimester, insulin needs rapidly increase from hPL secretion.
- Insulin needs continue to rapidly increase in the third trimester.
- Postpartally, insulin needs rapidly decrease to prepregnant levels.
Maternal and Fetal Effects
Effects may be minimal if diabetes is well controlled. There may be maternal and fetal newborn complications if the mother fails to control glucose levels.
| Mother | Baby |
|---|---|
| Infertility | Congenital anomalies |
| Spontaneous abortion | Polyhydramnios |
| PIH | Macrosomia (LGA) |
| Infections: moniliasis, UTI | Fetal hypoxia—intrauterine fetal death (IUFD), still births; increased perinatal mortality |
| Uteroplacental insufficiency | Neonatal hypoglycemia (common as soon as 1 hr after birth) |
| Premature labor | Prematurity |
| Dystocia | Respiratory distress syndrome (at 6th hrs. after birth) |
| More difficult to control DM— hypoglycemia/hyperglycemia | Hypocalcemia |
| Cesarean section is often indicated | |
| Uterine atony—postpartal hemorrhage |
Assessment Findings and Diagnosis
- History-Taking: family history of diabetes/gestational diabetes in previous pregnancy, previous macrosomic infant, previous infant with congenital defect or polyhydramnios, fetal wastage (spontaneous abortion, IUFD, stillbirth), obesity with very rapid weight gain, increased incidence of moniliasis and UTI, and marked abdominal enlargement (polyhydramnios and macrosomia)
- Signs of hyperglycemia: the three Ps of diabetes mellitus— polyphagia, polyuria, polydipsia.
- Weight loss from wasting due to ineffective glucose utilization
- Increased blood and urine sugar levels
Diagnosis is based on multiple tests:
- Screening: done at 24 to 28 weeks of gestation for those at risk:
- A 50 gram then 100 gram oral glucose solution is given for a 3-hr glucose tolerance test. Two abnormal values is considered as gestational diabetes mellitus (GDM) while one will place the woman on surveillance. Further information: OBG Project
- Glucose Tolerance Test (GTT): 100 gram GTT; commonly done between 28 and 34 weeks of pregnancy. The presence of two out of these four venous sample is considered an abnormal result:
- Fasting blood sugar: >105 mg/dL
- One hour after: >190 mg/dL
- Two hours after: >165 mg/dL
- Three hours after: >145 mg/dL
- Two-hour Postprandial Blood Sugar (PPBS): a result of 120 mg/dL or greater indicates abnormality.
Goals for Glycemic Control
- Fasting: <95 mg/dL
- 1-hr PPBS: <130–140 mg/dL
- 2-hr PPBS: <120 mg/dL
- Glycosylated Hemoglobin (HbA1c): a proportion of maternal hemoglobin found to be irreversibly bound to glucose, measuring long-term (3-month) compliance to treatment/glucose control. This value increases in hyperglycemia. The normal value ranges from 4% to 8%, with 6.5% being the cut-off point for diagnosing diabetes. This is also a useful test for diagnosing T2DM and for monitoring treatment.
- Urine glucose is not an accurate form of diagnosis because a pregnant woman will normally have glucosuria.
Nursing Management
- Early detection: take history, symptomatology, and prenatal screening.
- Encourage early prenatal management and supervision: frequent visits, maintaining diet, insulin use, serial ultrasonography, and hospitalization (for poorly controlled diabetes)
- Patient education: nature, effects, and signs and symptoms of DM; the rationale behind needing exercise, diet, and insulin for management; and danger signs and signs of infection to report.
- Promote control: one of the main reasons to control maternal glucose levels is to avoid stimulating the fetal pancreas, as the withdrawal of maternal glucose will result in neonatal hypoglycemia.
- Diet: the cornerstone of DM management and control; promote adherence to dietary regimen. (see table below)
- Exercise: decrease the need for insulin. 30 minutes of moderate-intensity aerobic exercise at least 5 days a week (minimum: 150 minutes per week) and walking after meals for 10 to 15 minutes is recommended. Excessive exercise can result in hypoglycemia. Exercise should be avoided if blood sugar is low or if the stomach is empty. Exercising should be done with a partner or someone to observe in case hypoglycemia occurs.
- Do not administer insulin into the extremity to be used for exercise, as this may accelerate absorption.
- Eat after prolonged exercise or physical activity.
- Always carry a diabetic ID.
- Insulin: oral diabetogenic agents are contraindicated.
- Insulin requirements increase in the second and third trimester, by as much as triple during the third trimester. In this period, the risk for ketoacidosis further increases.
- Regular and NPH insulin are used in pregnancy. Regular insulin is used during labor because long-acting insulins are not enough to prevent DKA.
- Regular insulin is the only insulin compatible with IV infusion
Diabetic Ketoacidosis (DKA)
Ketoacidosis may occur with poor compliance, infection, hyperemesis gravidarum, or diabetogenic drugs (corticosteroids, beta-sympathomimetic drugs). The risk associated with DKA in pregnancy is fetal ketosis— fetal distress, preterm birth, and perinatal mortality, making prompt recognition and treatment critical.
- DKA can be determined by blood sugar of >250 mg/dL, pH level of less than 7.3, serum bicarbonate of less than 15 mEq/L, and the presence of ketonemia or ketonuria.
| Content | Amount | Daily |
|---|---|---|
| Calories | 35 cal/kg EBW | 1,800 – 2,000 cal/day |
| Carbohydrates | 30% – 45% in 3 meals and 2 snacks for distributed consumption | 200 mg/day |
| Protein | 0.5–2 g/kg/BW | 70 g/day |
| Fats | Unsaturated |
- Encourage hospitalization for infection, regulation of insulin, assessment of fetal jeopardy, indications for early termination (ultrasound, urine/blood estriol levels, amniocentesis, phosphatidyl-glycerol, stress/non-stress tests)
- Early labor induction or cesarean section in the presence of fetal distress. Delivery ideally occurs around term, but is done earlier in cases of cephalopelvic disproportion (36/37 weeks) depending on lung maturity and fetal size.
- Continued monitoring: electronic fetal monitoring, left lateral recumbent positioning (supine hypotensive syndrome is worse with a larger fetus), fluid and electrolyte balance (D5W for glucose maintenance) with insulin titrated to maintain serum glucose levels between 100 and 150 mg/dL.
- Postpartum care: monitor the need for postpartal insulin. The need for insulin usually resolves a few hours after deliver, with IV insulin often discontinued at the time of delivery. A sharp increase in insulin requirement during the first 24 hours postpartum necessitates insulin dose monitoring and blood glucose monitoring.
- Encourage breastfeeding: breastmilk has an antidiabetogenic effect. However, the presence of acetonuria requires adjustment for insulin and diet before breastfeeding. Manual expression may continue to promote the diabetogenic effect of breastfeeding.
- Complications of the postpartum period:
- Hemorrhage from uterine atony (large fetus).
- Infections: candidiasis, UTI; avoid catheterization; provide meticulous perineal hygiene; instruct on the “front-to-back” technique of perineal flushing.
- Insulin Shock/Hypoglycemic Shock: observer for danger signs— diaphoresis, cold clammy skin, pallor, tremors, hunger. This often occurs during the peak action of insulin (2 to 4 hours after administration in regular insulin).
- Post-partum PIH: monitor blood pressure.
- Ensure return to normoglycemia with a GTT 4 to 12 weeks after delivery.
- Encourage contraception: reinforce physician’s recommendations— barrier (recommended), oral contraceptive pills (contraindicated due to decreased CHO tolerance), IUD (contraindicated due to infection)
Cardiac Disease
A variety of heart conditions, both congenital and acquired, that complicate pregnancy. These may include hypertensive disorders, hypercholesterolemia, myocardial infarction, cardiomyopathies, arrhythmias, valvular disease, thromboembolic disease, aortic disease, and cerebrovascular disease.
Risk Factors
90% of all cases are rheumatic in origin— rheumatic fever.
- Congenital defects of the heart
- Arteriosclerosis
- Myocardial infarction: pregnancy is generally contraindicated for clients who have experienced an MI before becoming pregnant and who have severe left ventricular damage and heart failure.
- Pulmonary diseases
- Renal diseases
- Heart surgery
- Advanced maternal age and preexisting co-morbid conditions have contributed to increased rates of maternal mortality
| Classification | Functional Capacity of the Heart |
|---|---|
| Class I | There is no limitation on physical activity; regular activities do not produce symptoms. |
| Class II | There is slight limitation; asymptomatic at rest, but regular activities produce palpitations, fatigue, dyspnea, and anginal pains. |
| Class III | There is marked limitation of activities; less than regular/ordinary activities cause symptoms. |
| Class IV | There is marked limitation of activities; symptomatic even at rest. |
Complications
Heart disease in pregnancy may result in congestive heart failure, maternal dysrhythmias, spontaneous abortion, premature labor, or intrauterine growth retardation.
Diagnosis
Nonspecific signs: palpitations, edema, tachypnea, fatigue, syncope, dyspnea, transient soft systolic murmurs, and elevated erythrocyte sedimentation rate (ESR) in the near term. The criteria required for establishing a diagnosis of cardiac disease in pregnancy include:
- Persistent diastolic or presystolic murmurs
- Permanent/unequivocal cardiomegaly
- Severe dysrhythmias
- Severe dyspnea prior to the stage of pressure on the diaphragm
- Loud, persistent systolic murmur
Cardiac decompensation is the point at which the heart can no longer compensate for the increased demands of the body, resulting in signs of decreased perfusion and fluid shifting:
- Moist cough
- Pedal edema; signs of pulmonary edema
- Dyspnea, increasing with minimal activity
- Tachycardia
- Chest pains on exertion
- Cyanosis
- Persistent heart murmurs
Further Evaluation
If severe dyspnea, syncope with exertion, hemoptysis, paroxysmal nocturnal tachycardia, and chest pain on exertion prompts further evaluation. An echocardiogram (ultrasound of the heart) and electrocardiogram (recording the heart’s electrical activity) may be used to evaluate heart function.
Treatment
Treatment requires early involvement of the cardio-obstetrics team to prevent maternal morbidity and mortality during the length of the pregnancy to the first year postpartum.
- Frequent prenatal visits and consultation with a specialist.
- Rest: physically and mentally depending on the functional ability of the heart. Being symptomatic may require bedrest. If stable, conservative management may be utilized.
- Digitalis, an inotropic agent, improves cardiac contractility but reduces cardiac rate. Check the woman’s heart rate before administering a dose; tachycardia or bradycardia warrants withholding of the dose.
- Antibiotics may be prescribed prior to the invasive procedure as a prophylaxis against rheumatic fever and as treatment for bacterial infections during pregnancy.
- Iron supplementation is used to treat or prevent anemia.
- Oxygen as necessary.
- Intrapartum goals: optimize perfusion— lateral position, analgesia, avoidance of hemorrhage, and avoidance of infection.
- Oxygen is delivered via mask as the parturient tends to mouth-breathe.
- Forceps or vacuum extraction may be used to avoid prolonged Valsalva maneuvers during the second stage of labor, but this commonly results in Bell’s palsy, warranting assessment.
- Elective CS may be done in some cardiac complications to avoid the strain of labor. However, the stress of major surgery, potential for infection, and increased blood loss are all taken into consideration.
Nursing Management
- Encourage early, regular, and frequent prenatal care/visits.
- Encourage compliance with therapeutic regimens:
- Decrease heart workload: rest, sleep (10 hours), avoid/treat anemia and infections, and prevent exhaustion, fatigue, and stress.
- Avoid activities that decrease oxygenation: smoking, overcrowded places, infection
- Avoid constipation: eat fruits and vegetables daily, have regular bowel movements, and exercise regularly. Walking is the best exercise.
- Observe proper nutrition: well-balanced diet, adequate protein, water, fruits, vegetables, low sodium, low fats, and low carbohydrates, and no junk food and stimulants.
- Report signs and symptoms promptly:
- Difficulty in breathing
- Shortness of breath with exertion or at rest
- Abnormal heart rate/rhythm: heart palpitations, rapid heart rate, irregular pulse
- Chest pain
- Bloody cough/coughing at night
- Early hospitalization
- Intrapartal Care:
- Thorough physical assessments: any change in cardiopulmonary status is promptly reported.
- Positioning: lateral, semi-recumbent (semi-Fowler’s) with hands and legs supported.
- Oxygen given by mask for mouth-breathing.
- Meticulous skin care, strict aseptic technique for preventing infection.
- Strict I&O monitoring: avoid fluid overload; observe NPO
- Provide psychological, emotional, and spiritual support for both the patient and family. Encourage the verbalization of concerns and provide thorough explanations of the care plan and progress of care to reduce stress and encourage cooperation and participation.
- Continuous cardiac monitoring for signs of cardiac failure and pulmonary edema is highly important; pulse rate is the most sensitive and reliable indicator of congestive heart failure. Report immediately if the pulse rate reaches over 200 BPM and the respiratory rate increases above 24 CPM. In this case, episiotomy and forces delivery may be indicated to shorten the second stage, and digitalis, diuretics, and antibiotics may be given as ordered.
- Postpartal Care: the reabsorption of placental circulation (sudden fluid overload) makes cardiac failure or decompensation likely in the early postpartal period. A rapid decrease in intraabdominal pressure following delivery also decreases vasocongestion and cardiac output rises.
- Monitor fluid balance: blood loss, I&O, and fluid flow rate.
- Assess frequently for signs of bleeding, sepsis, and CHF.
- Provide for nonstressful mother-infant interaction.
- Prove other typical care of a normal postpartum mother with provision for frequent rest periods.