The following discussion is based on a live discussion by Dr. Liela R. Ferrer, MD, PhD, MAED, CSPSH, FIAMS, FPASMAP, FPCGM.
Review of Anatomy and Physiology
The heart is the major circulatory organ of the body. It roughly weighs 300 grams and is divided between two general systems:
- Left Side: the part of the heart that pumps blood into systemic circulation.
- Right Side: the part of the heart that pumps blood into pulmonic circulation.
The heart is composed of four chambers and four valves:
- Right Atrium: receives blood from the superior and inferior vena cavae, being the terminal point of systemic circulation. Blood from this chamber passes through the tricuspid valve to move to the right ventricle.
- Tricuspid Valve: the valve connecting the right atrium and right ventricle.
- Right Ventricle: receives blood from the right atrium, and sends blood into pulmonic circulation through the pulmonic valve.
- Pulmonic Valve: the outlet connecting the right ventricle and pulmonary arteries.
- Left Atrium: receives freshly oxygenated blood from the pulmonic arteries, and sends blood into the left ventricular
- Mitral Valve: the valve connecting the left atrium and left ventricle.
- Left Ventricle: the most muscular chamber, as it is the chamber responsible for pumping blood out into systemic circulation.
- Aortic Valve: the outlet connecting the aorta and the left ventricle.
Blood Pressure
Blood pressure is the total pressure used to circulate blood throughout the body. It is calculated with (total peripheral resistance).
- Cardiac output is the total volume of blood pumped by the heart within one minute. The normal CO is 4 to 8 liters/min. It is the product of heart rate (number of strokes in a minute) and stroke volume (amount of blood pumped with one stroke).
- Stroke Volume has three principal components: (a) Preload, the amount of blood filling the blood during relaxation, i.e., the amount it stretches; (b) Afterload, the amount of blood left in the heart after contraction, which increases as resistance increases; and (c) contractility, the ability of the heart to contract.
- These volumes are all connected. In cases of vasoconstriction, total peripheral resistance increases. In cases of vasodilation, blood pressure, cardiac output, and resistance all decrease.
Abnormalities
- Hypertension is the elevation of blood pressure. Treatment uses vasodilators, which decrease cardiac output, preload, afterload, contractility, and total peripheral resistance.
- Shock results in decreased tissue perfusion from decreased blood flow. Treatment uses vasopressors/vasoconstrictors to raise cardiac output. Examples of this includes dopamine, dobutamine, livufed.
Blood pressure is measured as systolic over diastolic pressure. Systolic pressure is denoted by the first Korotkoff sound, produced by contraction of the ventricles. Diastolic pressure is the remaining pressure once the heart becomes relaxed and the ventricles refill.
Heart Sounds
The heart sounds are auscultated with a stethoscope. The diaphragm of the stethoscope is best for detecting S1 and S2, and the bell is best for S3, S4, and Murmurs.
- S₁ (Systole): the sound created by the closure of the atrioventricular valves (Tricuspid, Mitral). This creates the iconic “lub” part of the “lub-dub” sound of a heartbeat.
- S₂ (Diastolic): the sound created by the closure of the semilunar valves (Pulmonic, Aortic). This creates the iconic “dub” part of the “lub-dub” sound of a heartbeat.
- S₃ (Ventricular Gallop): an abnormal third heart sound heard in heart failure or volume overload as the ventricles fill rapidly.
- S₄ (Atrial Gallop): an abnormal fourth heart sound heard just before S₁. This sound is produced when an atrium attempts to send blood to a non-compliant or stiff ventricle, e.g., in hypertension, left ventricular hypertrophy, or aortic stenosis.
- Murmurs: the sound blood makes when flow becomes turbulent, such as in valvular heart disease (VHD).
Valvular Heart Diseases & Endocarditis
Valvular heart disease is any disease in which the valves of the heart become damaged, resulting in the inability of valves to close (regurgitation) where blood can flow backwards and impair circulation. This may also result in stenosis, where valves fail to open completely, limiting throughput. Both of these cause turbulent blood flow, which can be detected as murmurs auscultated with the bell of the stethoscope.
| Disorder | Sound & Character | Murmur |
|---|---|---|
| Mitral Stenosis | Rumbling; Low Pitch | Diastolic |
| Aortic Regurgitation | Blowing; Wide Pulse Pressure | Diastolic |
| Mitral Regurgitation | Blowing; High Pitch | Systolic |
| Aortic Stenosis | Harsh | Systolic |
| Mitral Valve Prolapse | Systolic Click | Systolic |
Murmur Types
Murmurs may be considered as diastolic murmurs— murmurs heard during diastole, or systolic murmurs— murmurs heard during systole. Additionally, a systolic click is found in mitral valve prolapse (MVP).
Monitor heart sounds, cardiac output, and signs of endocarditis. A 2D ECHO can be used to monitor the heart’s valvular structures and its contractions (ejection fraction). Surgical valve replacement may be done. Afterwards, anticoagulants are used to prevent thrombus formation.
Anticoagulants
This is a class of drugs that prevent the formation of blood clots. These include common examples such as heparin, warfarin, and enoxaparin. Other types of anticoagulants include:
- Oral antithrombin inhibitors (Dabigatran)
- Novel (new) oral anticoagulants (NOACs) such as Apixaban, Edoxaban, Rivaroxaban
Antidotes are used when bleeding related to anticoagulant use occurs. Normally, Protamine sulfate is used as an antidote for heparin (monitor PTT when in use) and Vitamin K is used for warfarin (monitor PT and INR when in use).
A common complication of VHDs is endocarditis. This is often caused by streptococcus viridans (normal gingival flora) and staphylococcus aureus. If endocarditis occurs, Penicillin G is the drug of choice as an antibiotic.
- As S. viridans is a major cause of native valve endocarditis, the patient teaching prioritized is to avoid vigorous brushing and to utilize an electric toothbrush rather than a manual one.
- As with all infection-prone diseases, maintain aseptic technique, especially when handling highly invasive contraptions such as central lines.
- Valvular heart disease is highly embolic. Among its severe complications are cerebral embolisms. Other visible manifestations such as Roth spots, Janeway lesions, and Osler nodes all manifest secondary to emboli. The patient should wear anti-embolic stockings if possible.
Embolus
Potential emboli are not massaged or manipulated to avoid dislodging them. A free-roaming embolus may become an pulmonary embolism or worse.
Pericarditis
An inflammation of the pericardial sac, a covering of the heart.
- Etiology: viral infection, Dressler’s syndrome (post-MI), neoplasms, renal failure, radiation, and connective tissue diseases.
- Clinical Findings: pain aggravated by inspiration is the most common symptom, and relieved with sitting or leaning forward (this differentiates it from MI). Infection results in leukocytosis, fever, and malaise.
- A common sign of pericarditis is a pericardial friction rub upon auscultation.
- ECG shows ST elevation.
- Nursing Diagnoses:
- Pain
- Risk of Decreased Cardiac Output
- Risk of Ineffective Breathing related to Pain
- Management: treat the cause of the pericarditis.
- Pain: NSAIDs, analgesics
- Monitoring for cardiac tamponade: diminished heart sounds, jugular venous distention, pulsus paradoxus, narrowed pulse pressure
- Medical Treatment: pericardiocentesis, aspiration of the pericardial contents if pericardial effusion occurs; dialysis is used if renal failure is the cause of pericarditis (uremia).
Pericardial Effusion
The pericardial sac normally only contains ~20 mL of fluid. In cases of inflammation, infection, or other disease processes, this fluid can accumulate and result in pericardial effusion. In severe cases, large volumes of fluid can cause cardiac tamponade. Heart sounds can become diminished, and a pericardial friction rub may be heard.
Heart Failure
Heart failure is the loss of function of the heart, being unable to pump blood out into pulmonic (right-sided) or systemic circulation (left-sided).
- Etiology: myocardial infarction, incompetent valves, cardiomyopathy (or any other disorders that affect the muscular layer of the heart).
- Right-Sided Heart Failure (RSHF) features a distended neck vein (backing up of the SVC), edema (congestion of systemic circulation), hepatomegaly (backing up of the IVC), and jaundice.
- Diet: low Na+, fluid limitation
- Left-Sided Heart Failure (LSHF) features pink frothy sputum, crackles, orthopnea (positional dyspnea), and paroxysmal nocturnal dyspnea from congestion of pulmonic circulation.
- Diagnostic Evaluation:
- CXR to visualize cardiomegaly
- 2D ECHO to evaluate decrease in ejection fraction (proportion of blood volume pumped out of the heart with each stroke) and increased CVP (for RSHF)
- Management: mn. 3Ds
- Diuretics to reduce pulmonary congestion. These include loop diuretics (Furosemide, Bumetanide) which lower serum potassium. Determine potential potassium imbalance in patients taking diuretics. The same caution is applied with potassium-sparing diuretics, which can result in hyperkalemia instead.
- Vasodilators reduce total systemic resistance, allowing the heart to pump better by reducing the preload.
- Digoxin, an inotropic, improves the contractility of the heart.
Digoxin
The therapeutic window of Digoxin is narrow, making it prone to toxicity. In normal use, it should remain between 0.5 to 2.0 ng/mL. Potassium is also a consideration for digoxin therapy— the receptors for digoxin are also receptors for potassium. If the patient has low potassium, the amount of open receptors for digoxin is greater, and poses a higher risk for toxicity than in normal patients.
Its signs of toxicity include:
- Anorexia, Nausea and Vomiting
- Blurred vision, green halos
- Bradycardia
- Nursing Management: monitor the client’s weight daily. A sign of failing circulation is the onset of edema, which results in sudden weight gain.
- Decrease the heart’s workload; provide periods of rest with any activity.
- Position the client in a semi-fowler’s or orthopneic position to facilitate breathing and circulation.
Coronary Artery Diseases
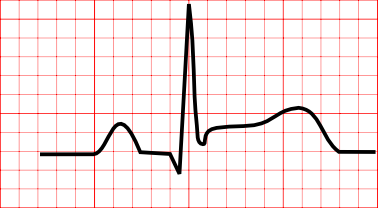
The aorta branches off into the right coronary artery and left coronary artery. The main problem involved with coronary artery diseases is atherosclerosis. It is the hardening or stenosis of vasculatures as a result of the build-up of plaque, and results in decreased perfusion. An imbalance between oxygen demand and supply produces ischemia, which can be visualized as ST depression in an ECG, which can eventually result in myocardial infarction, which can be visualized as ST elevation in an ECG.
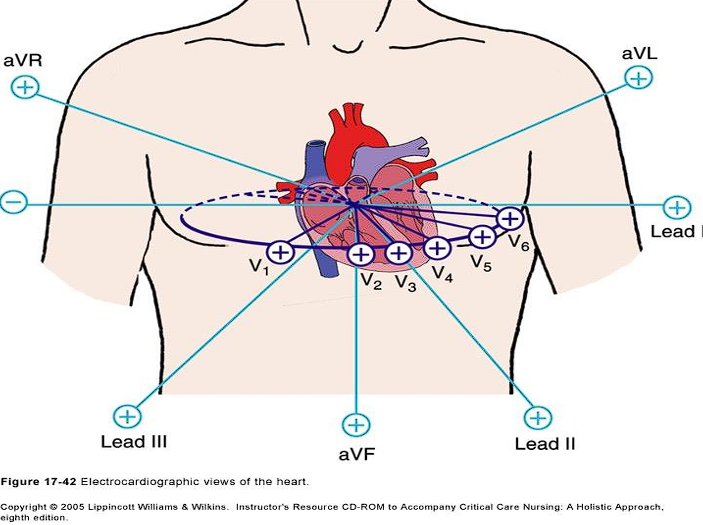
Lead Placement
The following are the corresponding leads to which wall of the heart is being detected:
- II, III, AVF: inferior wall
- I, AVL: lateral wall
- V1, V2: septal wall
- V3, V4: anterior wall
- V5, V6: lateral wall
- AVR: no specific view
Coronary Artery Sources
- The Right Coronary Artery supplies the inferior wall.
- The Left Coronary Artery supplies the anterior, septal, and lateral walls.
Unipolar Precordial Leads
- V₁: 4th ICS, Right Sternal Margin
- V₂: 4th ICS, Left Sternal Margin
- V₃: Midway between V₂ and V₄
- V₄: 5th ICS, MCL
- V₅: AAL on the same level as V₄
- V₆: MAL on the same level as V₄
Lead Axes
The two leads to consider for axis deviation is Lead I and Lead AVF. If both are positive, the axis remains normal.
Lead I Lead AVF Axis Positive Positive Normal Positive Negative Left Negative Positive Right Negative Negative Extreme Axis Deviation
Link to original
Read more about ECGs and their leads: Electrocardiography
Angina Pectoris
Angina pectoris is chest pain caused by hypoxia of the cardiac muscles. The pain is a substernal pain radiating to the left arm. There are different types of angina:
- Stable Angina: angina produced by exertion, and relieved by rest or the use of nitrates (nitroglycerin). The pain is predictable and consistent.
- Unstable Angina: angina that cannot be relieved by rest and nitrates, and progresses in severity and frequency. It is also known as a pre-infarction angina.
- Variant/Prinzmetal’s Angina: angina that appears most frequently during rest, caused by vasospasm.
Medications for Angina
- Nitrates: a vasodilator that reduces preload and afterload— commonly nitroglycerin. It is given at most three times every five minutes. It is delivered sublingually via spray or transdermally via patch. Nitroglycerin is photosensitive (place them in an amber container) and expire within six months.
- Beta-Blockers (-olols) (produces wheezing; given in caution to patients with COPD and asthma)
- Calcium Channel Blockers (-dipines, Verapamil, Diltiazem) (produces edema)
- Antiplatelets inhibit the aggregation of platelets. This is primarily aspirin, but can also be clopidogrel (Plavix) or dipyrimadole. Because of its nature, monitor the patient for bleeding.
- Anticoagulants as discussed earlier. Bleeding is also managed.
- Analgesics are used due to the pain experienced by the client. In myocardial infarction, morphine is used.
Myocardial Infarction
The death of the myocardial layer of the heart, most commonly caused by coronary artery disease. This is known as a heart attack.
- Risk Factors: non-modifiables such as race, age, gender; and modifiables (mn. SAHOD) smoking, (a) high chlosterol, hypertension, obesity, diabetes mellitus
- Dyslipidemia is an abnormal level of lipids in the blood. Normally, total cholesterol should remain under 200 mg/dL, triglycerides should remain under 150 mg/dL, and LDLs should remain under 100 mg/dL. HDLs, the “good cholesterol”, should be above 40 mg/dL.
- Clinical Manifestations: the main manifestation is crushing, substernal pain that may radiate to the jaw, neck, or left arm, which cannot be relieved by rest or nitroglycerin. Impaired perfusion results in cold, clammy skin; anxiety and a sense of impending doom; restlessness; and diaphoresis.
- Diagnostic Examination:
- ECG: an ST Elevation in an ECG reading is characteristic of myocardial infarction. Prior to injury, ischemia produces T-wave inversion and after injury, necrosis produces abnormal Q waves.
- Blood Tests: Troponin T, I (MI-specific), CKMB, Myoglobin (earliest), and Lactate Dehydrogenase (LDH; late to appear).
 4. Management: the MONA mnemonic (Morphine, Oxygen, Nitroglycerin, Aspirin) is apparently outdated, with only aspirin as remaining relevant and clearly beneficial for treatment. Aspirin is part of the reperfusion therapy necessary for recovering homeostasis in the coronary arteries. These include thrombolytics such as streptokinase. As usual, monitor for bleeding when using medications that reduce the clotting ability of the blood.
- If using morphine, Naloxone (Narcan) should be prepared in case of oversedation.
- The nurse assists in percutaneous transluminal coronary angioplasty (PTCA), where a balloon or stent opens up an occluded blood vessel and coronary artery bypass graft (CABG) surgery where an extra blood vessel (either saphenous vein, internal mammary artery, or radial artery) is used to bypass the occluded artery
4. Management: the MONA mnemonic (Morphine, Oxygen, Nitroglycerin, Aspirin) is apparently outdated, with only aspirin as remaining relevant and clearly beneficial for treatment. Aspirin is part of the reperfusion therapy necessary for recovering homeostasis in the coronary arteries. These include thrombolytics such as streptokinase. As usual, monitor for bleeding when using medications that reduce the clotting ability of the blood.
- If using morphine, Naloxone (Narcan) should be prepared in case of oversedation.
- The nurse assists in percutaneous transluminal coronary angioplasty (PTCA), where a balloon or stent opens up an occluded blood vessel and coronary artery bypass graft (CABG) surgery where an extra blood vessel (either saphenous vein, internal mammary artery, or radial artery) is used to bypass the occluded artery
Patient Teaching
Preoperatively, teach the client about the importance of avoiding vigorous coughing, performing leg exercises (embolus prophylaxis), and exercising incentive spirometry to maintain lung function. Postoperatively, monitor the client for signs of infection.
- Complications:
- Cardiogenic shock
- Arrhythmia: ventricular tachycardia, ventricular fibrillation— treated with defibrillation, except for ventricular tachycardia with pulse.
- Recurrent chest discomfort