Nursing is the diagnosis of human responses to actual and potential problems (American Nurses Association).
- The act of fulfilling the environment of the patient to assist him in his recovery (Florence Nightingale)
- To assist the individual, sick or well (Virginia Henderson)
Common Nursing Themes
- Nursing is Caring
- Nursing is an Art
- Nursing is a Science
- Nursing is Client-Centered
- Nursing is Holistic
- Nursing Adaptive
- Nursing is concerned with Health Promotion, Health Maintenance, and Health Restoration
- Nursing is a Helping Profession
Nursing, in contemporary times, is a profession. A profession is defined as a calling that requires special knowledge, skill, and preparation. Its primary characteristics include:
- Education: the nurse provides health teaching
- Theory: the nurse bases their actions on prefabricated theories and scientific knowledge.
- Service: the nurse provides service with a caring attitude, regardless of compensation.
- Autonomy: the independence of the nurse; the ability to exert judgments based on clinical expertise.
- Code of Ethics: the nurse guides their actions with the promulgated code of ethics to ensure quality, safe, and ethical care.
History of Nursing
- Intuitive Nursing (up to the 6th century): this dates back to primitive tribes where nursing was done with intuition rather than knowledge. It is rooted in compassion, superstition, religion, and magic.
- Apprentice Nursing (up to the 18th century): nursing starts to accumulate knowledge by way of schooling and apprenticeship. It was in this period that nursing schooling began, when Florence Nightingale became the most iconic nurse of all time. It may be considered as the golden age of nursing.
- Education Nursing: began with the Florence Nightingale School of Nursing opened at St. Thomas Hospital in London; the first formal education for nurses. This gave way to the proliferation of other nursing schools.
- Contemporary Nursing: present-day, professional nursing with the advent of modern machines and medical technologies.
Early Hospitals in the Philippines
| Hospital | Est. | Founder; Desc. |
|---|---|---|
| Hospital Real de Manila | 1577 | Gov. Francisco de Sande; for Spaniards |
| San Lazaro hospital | 1578 | Brother Juan Clemente |
| Hospital de Indio | 1586 | Charity-based through alms and contributions |
| Hospital de Aguas Santas | 1590 | Brother J. Bautista of the Franciscan Order |
| San Juan de Dios Hospital | 1596 | Brotherhood of Misericordia, administered by the Hospitallers of San Juan de Dios |
Notable Filipinos Nursing
- Josephine Bracken: installed a field hospital in an estate house of Tejeros, providing nursing care to the wounded night and day.
- Rosa Sevilla De Alvera converted their house into quarters for the Filipino soldiers during the Philippine-American War that broke out in 1899.
- Dona Hilaria de Aguinaldo: the wife of Emilio Aguinaldo, organized the Filipino Red Cross under the inspiration of Apolinario Mabini. She is the mother of the Philippine Red Cross organization.
- Dona Maria de Aguinaldo: the second wife of Emilio Aguinaldo, provided nursing care for the Filipino soldiers during the Revolution. President of the Filipino Red Cross branch in Batangas
- Melchora Aquino (Tandang Sora): nursed the wounded Filipino soldiers and gave them shelter and food.
- Trinidad Tiocson: “Ina ng Biac na Bato”, who stayed in the hospital at Biac na Bato to care for wounded soldiers.
Early Nursing Schools and Colleges
- Iloilo Mission Hospital School of Nursing (Iloilo City, 1906)
- St. Paul’s Hospital School of Nursing (Manila, 1907)
- Philippine General Hospital School of Nursing (Manila, 1907): the first hospital where a Filipino first occupied the position of chief nurse; Anastacia Giron-Tupas. The Superintendent Nurse of the Philippines.
- St. Luke’s Hospital School of Nursing (Quezon City, 1907)
- Mary Johnston Hospital and School of Nursing (Manila, 1907)
- University of Saint Thomas College of Nursing (1946)
- Manila Central University College of Nursing (1948)
- University of the Philippines College of Nursing (1948)
Socialization
Socialization is the process by which a person learns the ways of a group or society in order to become a functioning participant. (I’m not sure if the following section is categorized under this, but I didn’t see the correlation, so I’ll separate them for now.)
Patricia Benner’s Novice to Expert Theory
As presented by Patricia Benner (1984), there are five stages of proficiency for skills, knowledge, abilities, and values of nursing:
| Stage | Description |
|---|---|
| Novice | Student nurses with no clinical experience |
| Advanced Beginner | Marginally acceptable performance |
| Competent | Two to three years of experience; organizational ability, but lacking in speed and flexibility. |
| Proficient | Holistic clinical eye with long-term planning. The nurse focuses on the client rather than specific tasks. |
| Expert | The patient is autonomous, flexible, holistic, and highly proficient in providing care; the nurse is no longer reliant on rules, guidelines, or maxims to form an understanding. |
Nursing Roles
- Care Provider/Parent Surrogate: the role of the nurse concerned with recognizing the patient’s most immediate needs.
- Communicator/Helper: communicates with the client, supporting patients and colleagues. The end goal of communication is to establish trust.
- Teacher: the nurse provides health education by first assessing the learning needs of a patient, readiness of the client, then the actual provision of health teaching.
- Counselor: rather than providing advice, the nurse allows the patient to explore and formulate responses to their problems. The principal method used for this process is active listening; to offer the self and to let the client express their problems.
- Client Advocate: the nurse advocates and upholds the client’s rights.
- Change Agent: the nurse initiates changes and assists the client in making modifications in the lifestyle to promote health, to help the patient speak up for themselves. An important patient goal is to develop self-awareness.
- Leader: a mutual process of interpersonal influence through which the nurse helps a client make decisions in establishing and achieving goals to improve client’s well being.
- Manager: plans, give directions, develops staff, monitors operations, gives rewards fairly and represents both staff members and administration as needed.
- Researcher: participates in scientific investigation and uses research findings in practice.
- Collaborator: initiates nursing actions within the different disciplines of the health team such as physicians, dietitians, radiologists, respiratory therapists, etc.
Expanded Career Roles of Nurses
- Nurse Practitioner
- Clinical Nurse Specialist
- Nurse Anesthetist
- Nurse Midwife
- Nurse Researcher
- Nurse Administrator
- Nurse Educator
- Nurse Entrepreneur
- Dermatology Nursing
Focus of Nursing
- Health and Wellness Promotion: developing resources to maintain or enhance their well-being
- Illness Prevention: maintain optimal health by preventing disease.
- Health Restoration: helping people in improving health following health problems or illness.
- Care of the Dying: comforting and caring for people of all ages while they are dying.
In conducting nursing actions in conformance with the focus of nursing, there are four major concepts that a nurse must consider:
- Person: the recipient of the nursing care
- Health: the degree of wellness and well-being that a person experiences.
- Environment: the internal and external surroundings that affects a person.
- Nursing: attributes, characteristics, and actions of the nurse providing care in behalf of the client or in conjunction with the client.
Person
Differing approaches provided varying perspectives to human beings as individuals:
- Atomistic Approach: the man is an organism composed of organ systems, composed of organs, composed of tissues, composed of cells.
- Holistic Approach: the man is a unit of a system of society with interrelated and interdependent parts that function to produce a behavior; the man is more than the sum of his parts. The dimensions of man include:
- Man as a Social Being: an individual is able to relate with others; to socialize.
- Man as a Spiritual Being: an individual is capable of virtues such as faith, hope, and charity. They believe in a power beyond themself.
- Man as a Thinking Being are able to perception, cognition, and communication. They are capable of logical thinking and reasoning.
- Man as a Psychological Being are able to be rational. This allows for mercy, kindness, and compassion.
- Man as a Physical Being have such characteristics as genetic endowment, sex, and other physical attributes, structures, and functions.
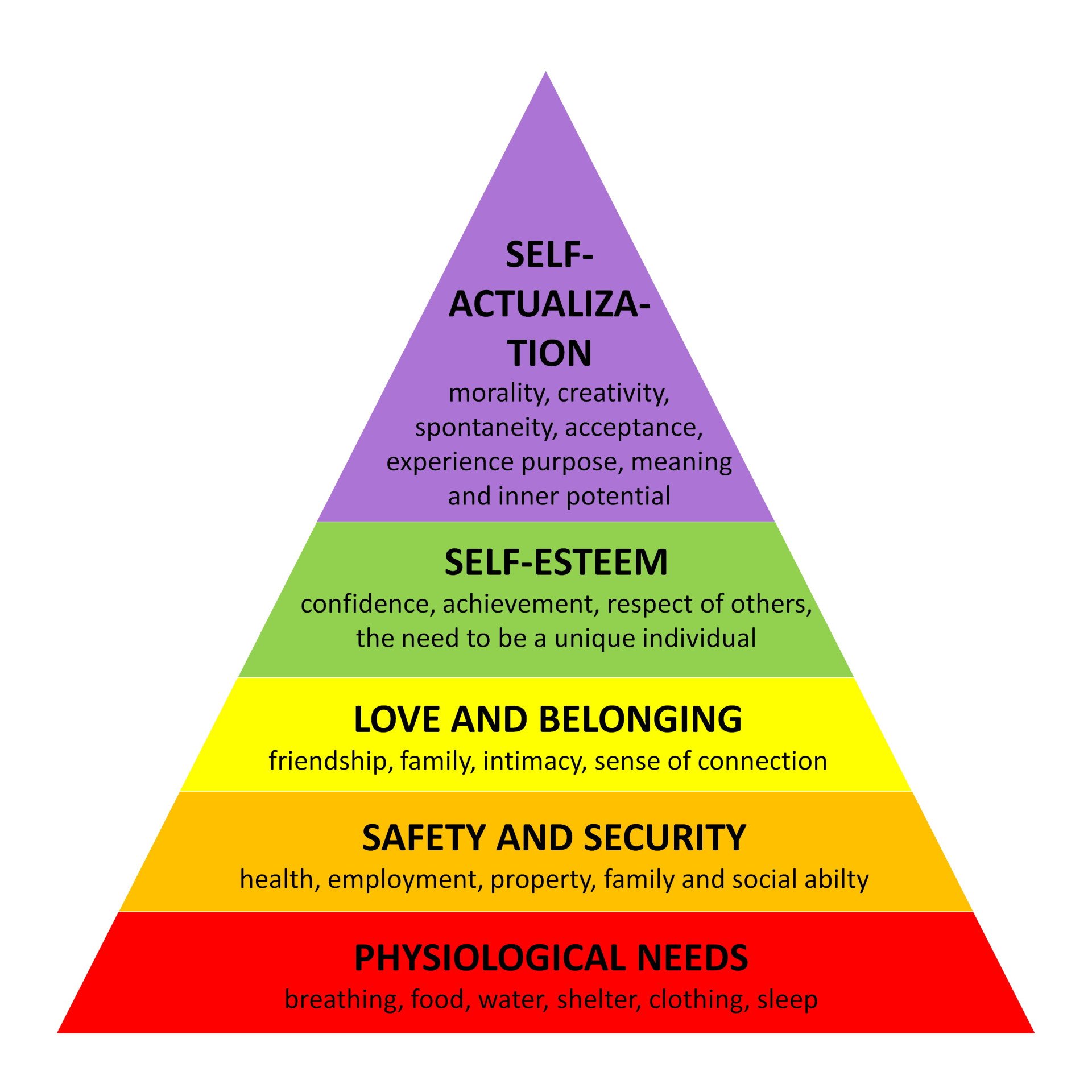
Hierarchy of Basic Human Needs
To preface, a need is some action, thing, or state that is essential to the survival of humans which, if absent, may lead to illness and, if fulfilled, can maintain or restore health. These needs are universal and interrelated, but may be deferred, may require stimulation from internal or external factors, and may be met in different ways. The prioritization of needs may be altered, but in general they are sequentially necessitated as postulated by Abraham Maslow (see next section).
Abraham Maslow’s Hierarchy of Needs is a sequential categorization of human needs, starting with:
- Physiological Needs (Biological Needs): those needs essential for the survival of the human being, e.g. oxygen, fluids, nutrition, temperature, elimination, shelter, rest, sex.
- Safety and Security (Psychological) Needs: physical safety (eliminate threats) and psychological safety (socialization; expectations of society).
- Love and Belongingness: the need to establish social relationships and to experience emotional nurturance and care to and from others.
- Esteem and Self-Esteem Needs: the desire for accomplishment, self-worth, strength, adequacy, competence, confidence, independence.
- Self-Actualization: the achievement of known potential; these individuals are excellent problem-solvers and communicators. They handle stress, critique, and suggestions well. They enjoy privacy and appreciate their self. They are content.
Health and Models of Health
Health is the fundamental right of every human being. It is a state of integration of the body and mind; a state of complete physical, mental, and social well-being, and not merely the absence of disease of infirmity (WHO). Other definitions of health from notable persons:
- Claude Bernard: Health is the ability to maintain the internal milieu. Illness is the result of failure to maintain the internal environment.
- Florence Nightingale: Health is being well and using one’s power to the fullest extent. Health is maintained through the prevention of diseases through environmental health factors.
- Walter Cannon: Health is the ability to maintain homeostasis or dynamic equilibrium.
- Imogene King: Health is a dynamic state in the life cycle. Illness is an interference in the life cycle.
- Sister Callista Roy: Health is a process of becoming integrated and whole as a person.
Wellness is a state of well-being. Well-being is a subjective perception of balance, harmony, and vitality. This appears in various dimensions:
- Physical: ability to perform tasks of daily living and achieve fitness of the different organ systems of the body.
- Emotional: stress-management and appropriate emotional expression.
- Social: ability to successfully interact with others, develop societal values, and to develop and maintain intimacy with significant others.
- Intellectual: learning and rational capability for personal, family, and career development
- Spiritual: purpose and fulfilment found in the belief of a higher power.
- Occupational: work-life/leisure balance.
Ecological Model
Leavell and Clark’s Agent-Host-Environment Model, simply known as the Ecological Model highlights three dynamic interactive elements that contribute to health and wellness:
- Agent: any environmental factor or stressor whether biologic, chemical, mechanical, physical, or psychological, whose presence or absence can lead to illness or death.
- Host: the person(s) who may be at risk of acquiring a disease based on family history of disease, lifestyle habits and age.
- Environment: all factors external to the host that may predispose the person to the development of disease.
Health Grid Model
Dunn’s Health Grid is a health grid in which a health axis and an environmental axis intersect, which demonstrate the interaction of the environment with the illness-wellness continuum.
- High-level wellness in a favorable environment. An example is a person who implements healthy lifestyle behaviors and has the biopsychosocial, spiritual, and economic resources to support this lifestyle.
- Emergent high-level wellness in an unfavorable environment. An example is a woman who has the knowledge to implement healthy lifestyle practices but does not implement adequate selfcare practices because of family responsibilities, job demands, or other factors.
- Protected poor health in a favorable environment. An example is an ill person (e.g., one with multiple fractures or severe hypertension) whose needs are met by the health care system and who has access to appropriate medications, diet, and health care instruction.
- Poor health in an unfavorable environment. An example is a young child who is starving in a drought-stricken country.

Health Belief Model
Becker’s Health Belief Model (1975) describes the relationship between a person’s belief and their health-related behaviors. It states that individual perceptions and modifying factors may influence health beliefs and preventive health behavior. These are the following:
- Individual Perceptions: perceived susceptibility, seriousness, or threat of an illness; how much the person believes they may become sick, and to what degree the illness will affect them.
- Modifying Factors: demographic variables, sociopsychologic variables, structural variables, and cues to action.
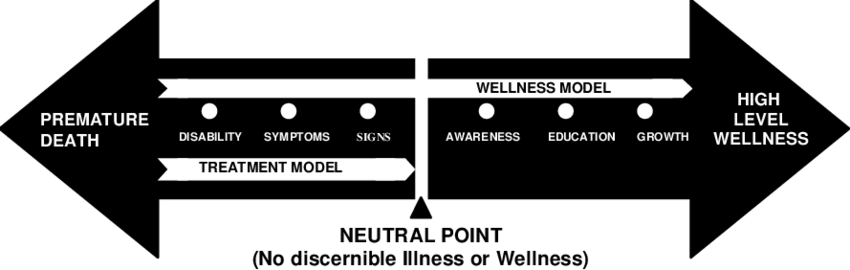
Illness-Wellness Continuum
Travis’ Illness-Wellness Continuum is a model that plots illness and wellness on a continuous axis rather than as distinct, discrete states of health. From the neutral point, moving to the right indicates health and well-being, and moving to the left indicates a decreasing state of health.
Smith’s Model of Health
Smith (1981) proposed multiple views of health organized into four distinct models to provide a holistic view on health of an individual:
- The Clinical Model defines health as the absence of any disease
- The Role-Performance Model describes health as the competent performance of socially defined roles
- The Adaptive Model characterizes health as a flexible adjustment to changing life situation; the individual is able to interact with the physical and social environment.
- The Eudemonistic Model views health as exuberant wellbeing; health is a condition of actualization or realization of one’s potential.
Disease and Illness
Disease is the alteration of functioning which results in the reduction of capacities and shortening of lifespan. Illness is a personal state in which the person themself feels unhealthy. Edward Suchman (1972) identified five stages of illness behavior:
- Stage 1: Symptom Experience; the person begins to believe that something is wrong. This involves three aspects— physical (fever, aching, malaise), cognitive (perception of the presence of illness), and emotional (stress and anxiety over illness)
- Stage 2: Assumption of the Sick Role: the persistence and progression of symptoms push clients to assume a sick role; a social phenomenon where individuals seek confirmation from social groups (family, friends) that they are ill and become exempted from normal duties and roles
- Stage 3: Medical Care Contact: after home remedies fail to remedy symptoms or they progress to a severe condition, individuals are motivated to seek professional health services. A real illness is validated, symptoms are explained, and outcomes are defined (reassurance or prediction).
- Stage 4: Dependent Client Role: the client depends on health care professionals for the relief of symptoms. Dependence makes the individual more passive and accepting.
- Stage 5: Recovery/Rehabilitation: the correction of symptoms, or adjustment to prolonged reduction in health and functioning in chronic illness.
Diseases may be classified depending on their nature:
- Etiology:
- Hereditary: defects in the genes of ascendants transmitted to the offspring.
- Congenital: defects in development potentially due to hereditary factors or teratogenesis.
- Metabolic: disturbances or abnormality in the metabolic systems of the body
- Deficiency: inadequate intake or absorption of essential dietary factors
- Traumatic: injury
- Allergic: hypersensitivity to physical or chemical stimuli.
- Neoplastic: abnormal or uncontrolled growth of cells
- Idiopathic: with an unknown cause, often self-originated and spontaneous
- Degenerative: degeneration of tissues and organs
- Iatrogenic: complications of treatment
- Presentation:
- Organic: diseases that result from physical changes in tissues or organs.
- Functional: diseases that occur without observable structural changes in tissues or organs; affects function rather than anatomy.
- Occupational: diseases resulting from exposure to hazards in the workplace environment.
- Venereal: diseases from sexually transmitted infections
- Familial: diseases running in families either due to genetic factors, lifestyle factors, or environmental factors.
- Epidemiology:
- Epidemic: a large number of individuals are affected at the same time.
- Endemic: a community that displays the presence of a disease continuously.
- Pandemic: an extremely widespread occurrence of disease spanning countries or continents.
- Sporadic: a disease with occasional cases not limited to one region.
General Risk Factors of Disease
- Genetic or Physiologic Predisposition
- Age
- Environment
- Lifestyle such as a sedentary lifestyle, substance use or abuse, etc.
- Sex
Levels of Prevention
- Primary Prevention: used in healthy individuals for the prevention of disease by reducing risk factors. This mainly comes in the form of health teaching.
- Secondary Prevention: used in potentially sick individuals (with S/S) for the early detection of disease. This mainly comes in the form of screening and testing.
- Tertiary Prevention: used in patients with disease (chronic, debilitative). The primary focus is on rehabilitation.
Communication
Communication is a process of transferring information and feelings between parties that can take the form of verbal (spoken, written) or nonverbal (gestured, paralanguage, etc.) communication. It consists of five basic components:
- Sender: the one to encode and deliver a message
- Message: the content of the communication
- Channel: the medium used for sending the message
- Receiver: the recipient of the message, and the one to decode the meaning of the message
- Response/Feedback: the reaction elicited by the message received.
As a quintessential element of nursing, communication requires specific characteristics in order to be considered effective and useful. These characteristics include:
- Simplicity: the message delivered is understandable to all parties involved, and uses simple straightforward delivery to concisely and efficiently convey its meaning.
- Clarity: the message spoken, written, or otherwise delivered, is clear, cohesive, and well understood. A message with conflicting meanings or appearance, or messages poorly written or enunciated are poor communicators of meaning.
- Timing and Relevance: messages are send in their appropriate time and should consider the client’s concerns and interests.
- Adaptability: the ability to adjust communication to consider circumstances and behavior.
- Credibility: the message transmitted is reliable and believed.
Organizational communication takes varying forms and methods based on the hierarchy employed in its delivery, and the context that it occurs in:
- Downward communication: managers transmit message down through the levels of management; traditional line of communication.
- Upward communication: employees provide input to their managers, who can pass it further up the administration hierarchy for decision.
- Lateral communication: “horizontal communication”; communication between departments on the same level of hierarchy. This is most frequently used to coordinate activities.
- Diagonal communication: communication between individuals or departments that are separate and not on the same level of hierarchy.
- Grapevine communication: an informal method of communication that naturally occurs (as if a vine growing) as clusters of individuals spend time together. This occurs outside of formal channels, such as the break room, through social media, etc.
The Nursing Process
Also read: The Nursing Process (by Ma’am Tuiza)
All activities of nurses follow the principles of the nursing process. It is the framework which allows nurses to use their knowledge and skills to provide care and help clients meet their needs. It is a systematic, rational method of planning and providing care using the process of ADPIE. It is characterized as:
- Systematic
- Skills and Knowledge-based
- Cyclical: the nursing process ends with evaluation, which evaluates both the interventions used and the outcomes achieved. This data can be used to stop, continue, or alter a care plan for patient care.
- Dynamic
- Client-centered
- Interpersonal and Collaborative: despite it being named the “Nursing Process”, it can be used to collaborate with other disciplines in delivering efficient, effective care.
- Universal
- Goal-oriented: the planning phase of the nursing process establishes goals and objectives of care that must be met for successful care.
- Priority-based: a patient can experience several or multiple health needs, and the nurse determines priorities to immediate needs in clients using the ABCs of Life, Maslow’s Hierarchy of Needs, and Client Preference.
Assessment
The process of collecting, organizing, validating, and recording data about a client’s health status. The data collected may be divided between subjective and objective assessment cues, depending on if the data collected is validated only by the patient (subjective) or if the data collected is observable or measurable.
Data Sources
Data may be collected from the primary (patient) and secondary (laboratory results, family statements, etc.)
- Initial Assessment: assessment done upon admission of the patient, including history-taking and assessment worksheets.
- Problem-Focused/Ongoing Assessment: continuing assessment done after admission for identified problems and risks of the patient, e.g., assessment done every four hours in the ward.
- Emergency Assessment: rapid (ABC) assessment during times of physiologic or psychologic crisis.
- Time-Lapse Assessment: assessment performed over two periods of time.
In an assessment, the nurse uses various methods for gathering data:
- Observation: the use of the five senses of the nurse to identify cues medically relevant.
- Interview: a planned and purposive conversation between the nurse and the client.
- Directive Interview (Structured Interview): a style of interview with optioned answers to elicit specific answers. These types of structures may be time-bound.
- Non-directive Interview (Semistructured/Unstructured Interview): a style of interview with no specific answers, best for allowing the client to verbalize their thoughts and feelings, letting the patient lead the conversation.
- Physical Examination: the implementation of IPPA, the four techniques of assessment.
- Inspection: visual inspection of affected body systems for abnormalities.
- Palpation: using the sense of touch to identify potential abnormalities.
- Percussion: the use of tapping to elicit a sound which may be heard as dull, resonant, hyperresonant, etc.
- Auscultation: auditory inspection of affected body systems (heart, blood flow in vessels, breath sounds, bowel sounds)
Distinctly, abdominal assessment utilizes IAPePa, as percussion and palpation may alter bowel sounds heard during auscultation.
Diagnosis
(a) Clustering and (b) analysis of data in order to (c) formulate a nursing diagnosis. Depending on the nature of the diagnosis, this may be
- Actual Diagnosis: a diagnosis signified by the presence of associated signs and symptoms about the client’s response to their health status.
- Risk Diagnosis: a diagnosis tackling the presence of risk factors or providing prophylaxis against future potential problems of the patient.
- Possible Diagnosis: an indication for the need of further assessment and data to determine the presence of a possible diagnosis.
- Wellness Diagnosis: a clinical judgment about the potential transition from one level of health to a higher level of health.
vs. Medical Diagnoses
Medical diagnoses identify the disease at hand, its pathology, and does not describe human responses. As long as the disease remains, this diagnosis does not change. In contrast, nursing diagnoses describe human responses to the disease process or health problem. These change throughout the disease process and can change frequently, and are limited to the scope of the nursing profession.
A nursing diagnosis can be composed of three components:
- Problem: the actual problem presented. This may be presented with quantifiers such as “Ineffective”, and “Risk for” that contextualize the patient.
- Etiology: the factors or causes related to the problem
- Signs and Symptoms: manifestations of the problem on the patient
Planning
A deliberate, systematic phase of the nursing process that involves (a) decision-making and (b) problem-solving skills. In involves:
- Establishing priorities
- Writing goals and outcomes and developing an evaluation strategy for the plan of care
- Selecting health care strategies/interventions
- Developing health care plans
- Communicating the plan of health care
| Type of Planning | Description |
|---|---|
| Initial Planning | Admission assessment that develops the initial comprehensive plan of care that is *initiated as soon as possible |
| Ongoing Planning | Occurs at the beginning of every shift or daily for determining required care for a nurse’s shift. It determines: - Changes in health status - Set priorities and decide problems to focus on - Coordinate the nurse’s activit |
| Discharge Planning | The anticipation and planning for client needs after discharge. Effective discharge planning begins at first client contact or admission. - Simple/Basic Discharge Plan: patient is sent home - Complex Discharge Plan: patient is referred to another institution an: |
Priority Setting
The process of establishing the preferential sequence or rank of interventions in accordance to the client’s most immediate needs.
Goals and Objectives are determined in the planning phase. The nurse declares the purposes and intentions that determines which interventions are relevant and used in the plan of care. These may be short-term (hours, days) or long-term (weeks, months) and follow the guidelines of:
- Client-centered: the goals must pertain to the client
- Realistic
- Collaborative: the interventions are compatible with the therapies of other disciplines providing care to the patient.
- Specific
- Behavior-focused: behavioral terms are used to pertain to the patient, rather than through purely physiologic goals of care.
- Measurable
- Time-bound
Once goals and objectives are established, interventions are planned. These interventions follow the directives of the goals set, and are classified according to the primary decision-makers:
- Independent Interventions: actions that the nurse is able to perform with their own discretion and clinical judgment.
- Dependent Interventions: actions dependent on the decisions of other healthcare professionals such as physicians.
- Collaborative Interventions: overlapping, shared function and responsibility among members of the healthcare team.
Implementation
Implementation is the phase of the nursing process where the health care plan is put into action. Before the actual performance of the planned interventions, the nurse:
- Reassesses the client to ensure that the interventions are still necessary, and to establish baseline data against which the effects of intervention is measured against.
- Set priorities for which interventions are to be performed immediately.
- The interventions can then be carried out and the procedures done, pertinent data obtained, patient status, and all other necessary information are documented.
What was not documented, was not done.
In carrying out interventions, delegation is an important method of increasing efficiency of care. It is the transfer of responsibility to a subordinate of the nurse (orderlies, nursing aides) to perform a task on behalf of the nurse. However, because of the specialized requirements of nursing responsibilities, strict guidelines are put in place to ensure that delegation will not result in error. The following segment is pulled from Atty. Luansing’s review on delegation:
Directing/Delegation
Delegation is a management function wherein a task, procedure, or obligation is done by another person who accepts it. Effective delegation is done by:
- Determine the task to be delegated. Tasks that are delegated are usually characterized as standard unchanging procedures.
- Choose a delegee to perform the task. It is the primary responsibility of the nurse to screen the delegee, provide proper instructions and tools needed, inform the scope of their duties and evaluate the result of tasks performed.
- Match staff competency with the task. There must be capacity and acceptance to perform the delegated task.
- Provide open and continuous communication with the delegee.
- Obtain constant feedback and evaluation from your subordinate during and after performing the task. As such, only tasks that the delegator can best perform, assess and evaluate may be delegated.
There are many principles and characteristics to follow for delegation to be effective:
Link to original
Provide a complete and continuous instruction for the delegated task.
Assume a face-to-face position and utilize proper eye contact when delegating.
Provide a calm environment when providing instructions.
Do not delegate during an emergency situation, as this should normally take time. Rushing delegation may result in errors and miscommunication.
Responsibilities may be delegated, but not accountability. Any errors by the delegee will be shared by the delegator.
Delegation should not breach confidentiality.
There must be a periodic and constant evaluation of tasks completed.
Give appropriate assistance and supervision.
Evaluation
Reassessment after the implementation of interventions to determine the acquisition of predetermined standards or outcome criteria. This phase appraises the extent to which goals and outcome criteria of nursing care have been achieved. The final judgment of the care provided can be summarized as:
- Goal Met, in which case, the cessation of the care plan or start of a secondary priority is done, and
- Goal Partially Met or Goal Not Met, in which case, alterations or extension of the care plan may be done
Evaluation does not only occur in after caregiving, but rather in three routines:
- Ongoing Evaluation: the patient is evaluated every day after procedures done.
- Intermittent: the patient is evaluated in a periodic, regular manner.
- Terminal: evaluation is done prior to discharge.
Quality Assurance
Evaluation of the provision of care is called quality assurance. It is a system put in place in order to assess routine care provided to maintain standards, and to increase the quality, efficiency, or effectivity where possible. This is targeted towards:
- Structure Evaluation: physical settings; the conditions wherein care is provided.
- Process Evaluation: technique; the manner utilized to provide care.
- Outcome Evaluation: consequence; the actual resulting health status as a result of the intervention.
Vital Signs
Vital signs are cardinal signs of the body that are assessed to provide a clinical picture of body functions.
Body Temperature
Body temperature is body heat resulting from heat production (primarily metabolism) and heat loss (conduction, convection, radiation, evaporation) in the body. This is measured in °C or °F ( , ).
- Core temperature refers to body temperature deep within the body, which remains relatively constant at around ~37°C. Surface temperature (commonly via axilla) refers to temperature of the skin down to the level of subcutaneous tissue. This fluctuates in response to the environment, ranging from 20°C to 40°C.
- Axillary Temperature: temperature taken from the axilla. Temperature readings normally range from 36°C to 37°C. The axilla should be dry (pat dry if necessary; do not rub as friction will elevate findings) and the bulb of the thermometer should sit in the center of the axilla.
- Clean the thermometer before and after use: remember the clean-to-dirty principle.
- Secure the thermometer in place— ask the patient to place their hand across the chest.
An abnormal elevation in body temperature is referred to as a fever; a febrile patient. A temperature higher than 37°C is called pyrexia, and a temperature higher than 40°C is called hyperpyrexia. Fevers can display a pattern in the appearance of fever:
- Intermittent: appearance and disappearance of a fever over the span of hours.
- Relapsing: appearance and disappearance of a fever over the span of days.
- Constant: a constant, minimally fluctuating fever.
- Remittent: a constant, widely fluctuating (≥2°C) fever.
A febrile patient must bring their temperature down gradually— through lysis. This is a normal drop in temperature associated with a better health status. However, a sudden drop of temperature to normal levels is known as a crisis (sudden defervescence) and can be an indication of hypothalamic impairment, as it is the thermoregulating center of the brain.
An abnormal decrease in body temperature is referred to as hypothermia. The processes involved in heat loss include radiation (no-contact transmission of heat), conduction (with-contact transmission of heat), convection (dissipation by air currents), and evaporation (evaporating water carry heat away from the body).
Factors Affecting Body Temperature
- Age: younger individuals have higher body temperatures; older individuals have lower body temperatures.
- Diurnal Variations: body heat during the day is higher than in the evening or early morning.
- Exercise: muscle activity increases body heat.
- Hormones: T₃, T₄, epinephrine, norepinephrine, and progesterone increase body heat. Estrogen decreases body heat.
- Stress: sympathetic nervous system stimulation increases hormonal activity (item 4) resulting in increased body heat.
Pulse
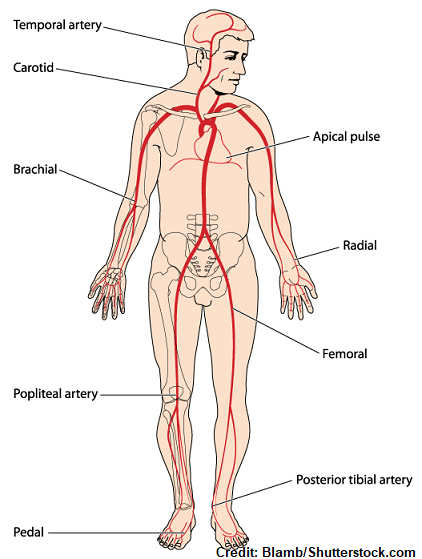
A pulse is a wave of blood created by the contraction of the left ventricle of the heart. It is detected in an individual through:
- Light to moderate palpation of arterial sites with two or three median fingers (not the thumb); strong pressure will obliterate the pulse.
- Auscultation at the point of maximal impulse (PMI); the apical pulse heard using a stethoscope.
Warm the hands before palpating the patient! The patient should rest for 15 minutes prior to assessment to ensure accurate findings.
An individual’s pulse is graded with many parameters on the different aspects of a pulse:
- Pulse Rate: the frequency of pulsation; the number of pulses in 60 seconds.
- This can be read as tachycardia, an abnormally increased pulse rate, or as bradycardia, an abnormally decreased pulse rate.
- Pulse rate is affected by many factors: age (see table below), sex (↑ in men), exercise (↑ PR), fever, hemorrhage, stress (↑ PR), postural changes (↑ PR), and medications (increase or decrease depending on medication given)
| Age Group | Bradycardia | Normal | Tachycardia |
|---|---|---|---|
| Infant | <100 | 120 | >140 |
| Toddler | <90 | 110 | >130 |
| Preschooler | <80 | 100 | >120 |
| School-age | <70 | 90 | >110 |
| Adult | <60 | 80 | >100 |
- Peripheral Pulses: pulses auscultated or palpated from peripheral sites of the body
- Apical Pulse: the strongest pulse found at the 4th to 5th intercostal space on the left midclavicular line
- This is more reliable in determining heart rate because of its proximity to the heart; a peripheral pulse may display a pulse deficit, a difference between peripheral pulse rate than an apical pulse rate.
- Amplitude: the strength of the pulse graded qualitatively:
- 0: absent
- 1: weak and thready
- 2: normal
- 3: bounding
- Pulse Rhythm: the interval between pulses. In a normal individual, rhythm remains constant and continuous; an abnormal rhythm is found in irregular beating patterns of the heart called arrhythmia.
Respiration
The act of breathing. The primary respiratory center is the medulla oblongata, which maintains breathing at a respiratory rate (RR) of around 16 to 24 breaths per minute.
- Costal/Thoracic Breathing: breathing that expands the chest, common in adult clients
- Diaphragmatic/Abdominal Breathing: breathing that expands the abdomen
Descriptors or aspects of respiration:
- Inhalation: inflow of air
- Exhalation: outflow of air
- Ventilation: physical movement of air in and out of the lungs
- Hyperventilation: deep, rapid breathing
- Hypoventilation: slow, shallow breathing
- Hypoxia: decreased oxygen in tissues
- Hypoxemia: decreased oxygen in the blood
- Asphyxia: inability to breath with an intact respiratory system
- Eupnea: normal breathing; quiet and effortless
- Apnea: cessation of breathing
- Tachypnea: rapid breathing (>24 breaths/min)
- Bradypnea: slow breathing (<12 breaths/min)
- Dyspnea: difficult, labored breathing
- Orthopnea: breathing is difficult in non-upright positions
Factors Affecting Respiration
- Exercise (↑ RR)
- Stress or emotional arousal (↑ RR)
- Environmental factors (e.g., higher temperature raises RR, higher altitudes raises RR)
- Medications. Notably, narcotics depress respiration; oversedation can result in respiratory arrest such as in medullary anesthesia.
Breath Rhythms
Similar to pulse rates, breathing also has rhythms that occur in normal and abnormal breathing:
- Cheyne-Stokes Breathing: waxing and waning from very deep to very shallow breathing with periods of apnea.
- Biot’s Breathing: shallow breathing with periods of apnea.
- Kussmaul’s Breathing: deep, rapid breathing associated with acidosis (the body attempts to expel carbon dioxide to regulate pH)
Breath Sounds
| Normal Breath Sound | Description | Found At |
|---|---|---|
| Tracheal | Harsh breath sounds | Level of the trachea |
| Bronchial | High-pitched breath sounds | Level of the bronchi |
| Bronchovesicular | Medium-pitched breath sounds, a blowing sound of air moving through larger airways | Level of the scapula (mid-lung field) |
| Vesicular | Low-pitched breath sounds, a gentle sighing sound. | Level of the lower lobes of the lung |
| Abnormal Breath Sound | Description |
|---|---|
| Crackles/Rales | Popping sounds heard from fluid filling the alveoli; crackles are a coarser form of rales. |
| Stridor | Harsh sounds (wheezing) heard upon inhalation |
| Wheezes | High-pitched, whistling sounds as air passes through narrowed airways upon exhalation |
| Pleural Friction Rubs | Grating, scratching sounds heard from friction between inflamed pleura. |
Blood Pressure
The pressure exerted by the blood as it pulsates through the arteries. It is measured in millimeters of mercury (mm Hg) and is measured as two values: systolic (contractile) pressure and diastolic (relaxed) pressure:
- Systolic pressure is the pressure of blood during contraction of the ventricles.
- Diastolic pressure is the pressure of blood in between heartbeats; at rest.
- Pulse pressure is the difference between diastolic and systolic pressure. This is normally 30 to 40 mm Hg.
Procedure
- Prepare the client for assessment. They should be at rest for at least 30 minutes. At assessment, the patient is positioned neutrally in a standing, sitting, supine, or Fowler’s, with the arm at the level of the heart. The left arm is preferred due to its proximity to the heart, but contraindications may be in place, such as: extremities with intravascular infusion, blood transfusion, arteriovenous fistula, burns, trauma, casting, bandaging, or the arm on the side of a mastectomy or lymphadenectomy are all contraindications for blood pressure assessment.
- Prepare the equipment for assessment.
- The cuff should be fit just right; not too tight (will give high readings) or too loose (will give low readings); it should cover at least two-thirds of the limb circumference. When placed, the cuff is positioned one inch (2.5 cm, two fingerbreadths) above the antecubital space.
- Fully deflated; calibrated to 0 when not in use. No leaks should be present.
- Non-disposable cuffs may become significantly contaminated— clean cuffs according to institutional standards.
- In initial examination, perform a palpatory determination of systolic pressure to give an estimate of systolic pressure:
- The brachial artery is palpated for a thrill
- Inflate the cuff until a thrill is no longer palpable— this is the estimated systolic pressure, and guides the initial pressure used when inflating the cuff.
- Deflate the cuff. Further assessments should be done after one to two minutes.
- Position the stethoscope above the brachial pulse. The preferred side used is the bell for listening to the Korotkoff sounds that dictate the systolic and diastolic readings.
- Inflate the cuff until 30 mm Hg above the palpated systolic blood pressure, then deflate the cuff at a rate of 2 to 3 mm Hg/s.
- Watch the sphygmomanometer for the reading, and listen for the reappearance of a bruit (mark as systolic blood pressure) and the disappearance of the pulsating sound (mark as diastolic blood pressure).
- If abnormal, both arms should be checked and compared. The higher blood pressure is recorded. A difference of no less than 100 mm Hg should be present.
Pain
Pain is an unpleasant sensory and emotional experience associated with the actual or potential tissue damage, or described in terms of such damage or both.

Pain comes in many presentations, and is highly subjective. Sources of pain for one person may not be a source of pain for another. Pain may be described as:
- Acute: pain lasting for up to six months, appearing suddenly or slowly. Severity covers all level of pain from mild to severe.
- Chronic: pain lasting for six months or longer. These individuals adapt and lose the behaviors associated with patients in pain.
- Radiating: pain extending from the damaged tissues to other parts of the body.
- Referred: pain felt in a body part disconnected from the damaged tissues producing pain.
- Intractable: pain highly resistant to relief, e.g., in acute compartment syndrome.
- Phantom: a painful sensation perceived in a missing body part.
Pain Guide Questions (PQRST)
- Precipitating or Palliative: what causes or relieves the presenting symptoms?
- Quality or Quantity: How severe are the symptoms? How does it look, feel, or sound?
- Region or Radiation: where is pain found? Does the pain spread or radiate anywhere?
- Severity Scale: how bad is the pain on a scale from 1 to 10?
- Timing: when was the onset, what is the duration, and how often does pain occur?
Infection
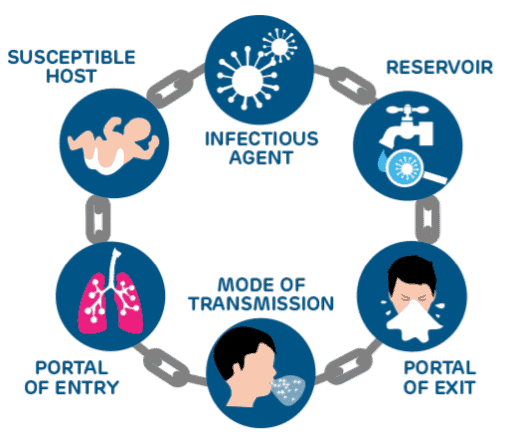
An infection is a disease state that results from the presence of pathogens in or on the body. The chain of infection is a series of components that are necessary in the spread of infection across hosts:
- Infectious Agent: the pathogen itself. This consists of bacteria, viruses, parasites, or fungi.
- Reservoir: an environment where a pathogen thrives; organisms, soil, water, etc. where microorganisms are free to grow and multiply.
- Portal of Exit: a method by which the infectious agent leaves its reservoir such as in feces, blood, mucus, etc.
- Mode of Transmission: a medium by which the free infectious agent is dispersed. This is classified as:
- Contact Transmission: transfer from person-to-person by contact such as touching, kissing, and sexual intercourse. This may also be indirect, involving a fomite (inanimate object) touched by the infected person then a susceptible host.
- Vehicle Transmission: water, food, air contamination
- Vector Transmission: mechanical or biological vectors
- Portal of Entry: a passage by which an infectious agent enters another organism. This is commonly in the form of a break in the skin, nose, mouth, or mucus membranes.
- Susceptible Host: an organism susceptible to pathogenesis by the infectious agent. In humans, this includes those in the extremes of age and those who are immunocompromised due to a disease or as a condition.
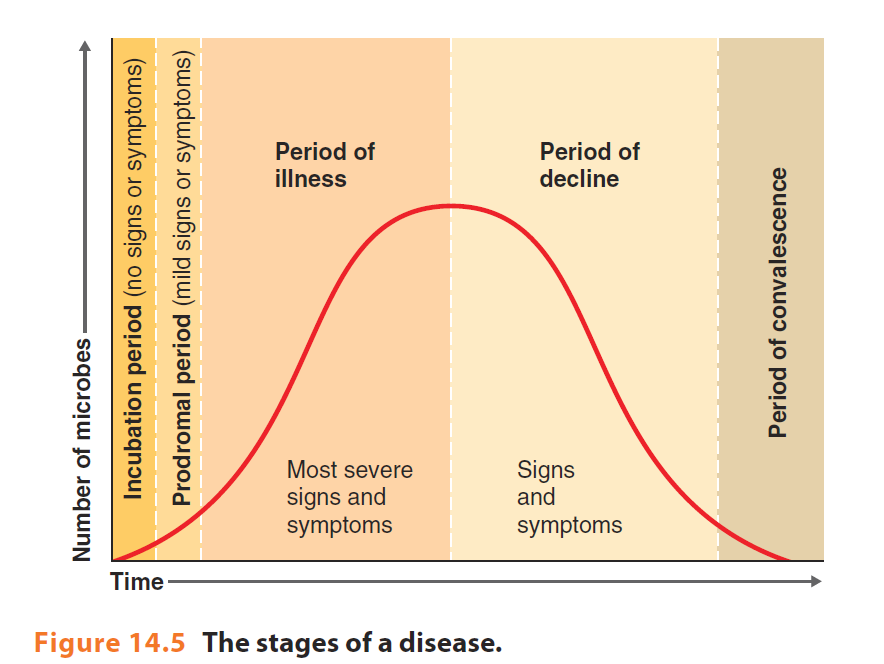
Stages of Infection
- Incubation Period: the interval between the invasion of a pathogen to the appearance of symptoms. The pathogen is incubated— it grows and multiplies.
- Prodromal Stage: the onset and experience of symptoms, lasting from several hours to days. Signs and symptoms are often vague and non-specific, such as fatigue, malaise, and a low-grade fever. This is the most infective stage.
- Full Stage of Illness: specific signs and symptoms appear; the illness produces full-blown disease.
- Convalescent Stage: the recovery period from infection, where signs and symptoms disappear and the person results to a pre-disease or otherwise healthy state.
Disinfection and Asepsis
To be continued