Sources
This discussion summarizes multiple presentations produced by Ma’am Tuiza.
The Nursing Process, a systematic scientific method of formulating and providing nursing care generally consists of five core steps, summarized by the mnemonic ADPIE. In order, they are Assessment, Diagnosis, Planning, Intervention/Implementation, and Evaluation.
Assessment
Assessment is the first step of the nursing process. There are four major activities to do during the assessment phase: collection, organization, validation, and documentation of data. Assessment aims to determine client health status prior to, during, and after nursing and medical interventions. Assessment can be done in various settings, and can by typed as such:
| Based on Timing | Function |
|---|---|
| Initial Assessment | Done after admission to establish a complete database for problem identification, reference, and future comparison. |
| Problem-Focused Assessment | Ongoing process integrated with nursing care to determine the status of a specific problem identified in an earlier assessment. |
| Emergency Assessment | Done during any physiologic or psychologic crisis of the client to identify life-threatening, new, or overlooked problems. |
| Time-Lapsed Reassessment | Done several months after initial assessment to compare the client’s status to baseline data previously obtained. |
| Based on Focus | Function |
|---|---|
| Comprehensive Assessment | A complete assessment and health history performed upon admission. |
| Focused Assessment | Assessment focused on a particular need or healthcare problem. |
| Ongoing Assessment | Systematic monitoring and observation related to specific problems. |
Data Collection
This function of assessment aims to gather information about a client’s health status. The end goal product of this step is to produce a database, which contains all the information about a client. This process aims to be systematic and continuous to prevent the omission of significant data and to reflect a client’s changing health status. There are various categories of data collected:
- Nursing Health History
- Biographic Data
- Chief Complaint
- Past History: illness, immunization, allergies
- Family History of Illness
- Lifestyle: personal habits, diet, sleep pattern
- Social Data: ethnic affiliation, educational and occupational history
- Psychologic Data: stressors, coping pattern
- Patterns of Healthcare: ophthalmologist, gynecologist, dentist
- Physical Assessment
- Primary Care Provider’s History
- Physical Examination
- Results of Laboratory and Diagnostic Tests
- Material Contributed by Other Health Personnel
Data Types
| Data Type | Description |
|---|---|
| Subjective Data | Symptoms felt by the patient, which can only be described or verified solely by the patient. These are covert data such as itching, pain, feelings of worry, feelings, values, beliefs, and attitudes. |
| Objective Data | Signs observed or measured by the examiner, often tested against accepted standards. These are overt data such as discoloration of the skin, blood pressure, vital signs, etc. |
| Constant Data | Data that do not change over time such as ethnicity and blood type. |
| Variable Data | Data that is subject to change over time, even acutely, such as that of pain, blood pressure, and height. |
| Primary Data | Data obtained directly from the client or source. This is often the most reliable source. |
| Secondary Data | Data obtained anywhere other than from the client. All secondary sources should be validated when possible. This includes family members or other support persons, health professionals, records, and reports. |
Data Sources and Collection Methods
- Client: usually the best source of data except in cases of illness, young patients, or patients too confused to communicate clearly. Some clients cannot or do not with to provide accurate data. In these cases, family members or significant others can be sources of secondary data.
R.A. 10173: Data Privacy Act of 2012
You can remind the client of Data Privacy if they are hesitant about the safety of their information. The Data Privacy Act mandates the protection of all privileged client information from those not involved in their care. Additionally, the Nurses Code of Ethics and Patients’ Bill of Rights place privacy and confidentiality as important aspects of data handling.
- Support People: family members, friends, and caregivers who can give information on the client’s response to illness, the client’s stressors, family attitudes on illness and health, and the client’s home environment. As mentioned, they are especially important for very young, unconscious, or confused clients. Information, if obtained from support systems, should be notated as such.
- Client Records: documented information by various healthcare professionals, including medical records, records of therapies, and laboratory records.
- Healthcare Professionals: nurses, social workers, and primary care providers can share information to ensure the continuity of care when clients are transferred to and from home and healthcare agencies.
- Literature: professional journals and reference texts can be used as basis for care. Literature needs to be reviewed when used, including the comparison of findings to the current standards, comparison to cultural and social health practices, spiritual beliefs, and the assessment data needed for specific client conditions.
The nurse is able to obtain data with three main methods:
- Observing: the nurse utilizes their senses and specialized knowledge to obtain data about the patient. The process of observation is systematic to avoid oversights:
- Clinical Signs are checked, particularly of distress. This includes pallor, labored breathing, and behaviors indicating pain.
- Threats to Safety are determined, including both present and foreseeable risks. A common example of this is a lowered siderail.
- Equipment are also maintained and checked if they are properly functioning and configured. Examples include IV sets, oxygen tanks, monitors, and ventilators.
- Environment: many environmental factors can affect health and quality of life. Even minor, non-lethal factors such as lighting, cleanliness, and the people in the client’s immediate environment are considered.
| Sense Used | Client Data Obtained |
|---|---|
| Vision | Overall appearance (body size, posture, grooming) Signs of distress or discomfort Facial and body gestures Skin color and lesions Religious or cultural artifacts (books, icons, candles, beads) |
| Smell | Body or breath odors, especially in discharges and wounds. |
| Hearing | Lung and heart sounds Bowel sounds Ability to communicate Language spoken Orientation to time, person and place |
| Touch | Skin temperature and moisture Muscle strength (via hand grip) Pulse rate, rhythm, and volume Palpable lesions (lumps, masses, nodules) |
- Interviewing: communication planned and carried out with a purpose, such as for a nursing health history. Two common approaches are used: direct (highly structured, specific) and non-directive (rapport-building, the client is allowed to control the purpose, subject matter, and pacing).
- Closed Questions: short, direct questions seeking factual answers. “What medications have you taken today?” “Are you having pain now?”
- Open-ended Questions: questions that elaborate, clarify, or illustrate their thoughts or feelings. Non-directive. “How have you been feeling lately?” “What brought you to the hospital?”
- Neutral Questions: open-ended, non-pressuring questions. Non-directive. “How did you feel about that?” “What do you think led to the operation?”
- Leading Questions: questions that direct client answers. Directive. “You will take your medicine, won’t you?” “You’re stressed for the upcoming surgery, aren’t you?”
Planning an Interview
An interview should be planned according to:
- Time: the client should be comfortable and free of pain, with little opportunity for interruptions.
- Place: well-lit, well-ventilated rooms that are free of noise and distractions should be used as much as possible.
- Seating Arrangement: the nurse positions themselves at a 45° angle to the bed. This makes it more familiar than sitting behind a table or standing at the foot of the bed, while maintaining a professional distance.
- Distance: an appropriate distance of 2 to 3 feet is used during an interview.
- Language: the nurse takes care to convert medical terms to common language; at the level of the client’s educational attainment.
- Flow: the interview consists of an opening (introduction, rapport, orientation), body (questioning, answering), and closing (clarifications, conclusions/summary, termination, and future planning if necessary).
- Physical Examination: the application of inspection, palpation, percussion, and auscultation (mn. IPPA), carried out systematically, often in an organized (head-to-toe; cephalocaudal, and body systems approach).
Organizing Data
Nurses organize data in a written or electronic format to systematically organize assessment data. A common framework for organization was made by Marjory Gordon as Gordon’s 11 Functional Health Patterns:
| Functional Health Pattern | Contents |
|---|---|
| Health Perception and Health Management | General health, health promotion activities, general health appearance, attitudes toward medical advice. |
| Nutritional-Metabolic Pattern | Typical intake, changes in weight, appetite, wound healing (well or poor), skin lesions, dental problems. |
| Elimination | Excretion patterns that need to be evaluated, such as constipation, incontinence, and diarrhea. The excretion itself should also be examined for color and consistency. |
| Activity-Exercise | Whether one is able to perform daily activities normally without any problem. This includes feeding, bathing, toileting, dressing, grooming, etc. There are generally four levels of functionality: - Level I: requires equipment/device use. - Level II: requires assistance or supervision from another person. - Level III: both I and II - Level IV: is dependent and does not participate. |
| Cognitive-Perceptual | Neurological function; the person’s ability to comprehend information. This includes hearing, vision, memory, decision-making, learning, etc. |
| Roles-Relationships | Family conditions, problems, dependencies, etc. Only obtained if necessary for the patient’s age and specific situation. |
| Self-Perception/Self-Concept | How does the patient describe themself? Self-image, satisfaction with the self and/or body (esp. after illness or disability), etc. |
| Coping-Stress | Any stressors, persistent stress/anxiety levels, the use of medications, drugs, or alcohol. Commonly used coping mechanisms and their success are recorded. |
| Value-Belief | Religion, spirituality, future plans, etc. The most important consideration is if religious practices may interfere with healthcare or vice versa. |
| Medication and History | The patient’s health history, medication history, and current medication regimen. |
| Nursing Physical Assessment | Biophysical data, vital signs, etc. |
Validating Data
Data, as much as possible, and especially secondary data, is validated to ensure accuracy; basically, double-checking the data to ensure accuracy. Generally, data can be considered as cues which are signs and symptoms, and inferences, which are further interpretations and conclusions based on the cues.
Faulty inferences can result from jumping to conclusions or focusing in the wrong direction.
There are some types of data that do not require validation. These include things such as height, weight, birth dates, and most laboratory studies. However, those that do require validation are data that need to be correlated with the client’s physical or emotional behavior, and data found to have discrepancies obtained in the nursing interview (subjective data) and the physical examination (objective data), or when the client’s statements shift between assessments. The following are examples of validating data:
- Comparing subjective and objective data: the statement of “I’m feeling hot” warrants the nurse to check the patient’s body temperature.
- Clarify statements: statements are clarified if they are ambiguous or vague. “I felt sick on and off for six weeks” warrants the nurse to clarify: “Describe what your sickness is like. What does on and off mean?”
- Cues, not inferences: data is based on cues and not inferences. For example, the observation of dry skin and poor skin turgor (tenting) produces an inference of dehydration. Furthermore, additional data is obtained to support any inferences made, if necessary. In the previous example, the nurse would then obtain data on the client’s fluid intake, amount and appearance of urine, and blood pressure. If these also correlate as signs of dehydration, the inference is strengthened.
- Double-check abnormal data: all abnormal, especially those of extreme abnormality, is double checked. For example, an abnormal blood pressure reading of 210/95 mm Hg is double-checked with another sphygmomanometer and/or by another nurse.
- Check for interference: many factors can interfere with accurate measurement. The nurse checks for potential sources of abnormality before measuring. For example, a crying infant will often display an abnormal respiratory rate. In this case, the finding is not representative of the infant’s actual respiratory status, and quieting of the infant is required before an accurate assessment can be made.
- Use references: phenomena may be explained using information from reputable textbooks, journals, and research reports. For example, a geriatric patient with a tiny purple/blue-black swollen area under the tongue is normal according to literature stating such physical changes (sublingual varices) are normal with aging.
Documenting Data
The nurse completes assessment by recording client data. All data are recorded factually rather than interpretatively. This data can be used for the following steps of the nursing process, and should not change in meaning when written down. For example, a client’s morning meal is recorded literally: “Client consumed 240 mL coffee, 120 mL juice, 1 egg, and 1 slide of toast” rather than “Client appetite is good.” (a judgment)
Diagnosis
Nursing diagnosis entails problem identification. It is a clinical judgment about the client’s responses to actual and potential health problems or life processes. It is based on critical analysis of assessment data and identified client strengths and problems. In contemporary standards, the North American Nursing Diagnosis Association (NANDA) for nursing diagnoses. A nursing diagnosis can focus on different types of problems:
| Type | Description |
|---|---|
| Actual nursing diagnosis | Problem-based. A problem present at the time of assessment. Ex.: “Altered respiratory status”, “Impaired ability to cope” |
| Health promotion diagnosis | Client preparedness to improve health condition. Ex.: “Willingness to learn about the health maintenance”, “Willingness to change health practices” |
| Risk nursing diagnosis | Problem-based, for problems not yet present but whose risk factors are present. Ex.: “Risk for or Potential for impaired breathing patterns” |
| Syndrome diagnosis | Syndromes are a set of similar nursing diagnoses that occur together, and can be resolved with similar interventions. Ex.: “Chronic Pain Syndrome” |
| Wellness diagnosis | A state of health that may be further enhanced by health promoting activities. Ex.: “Readiness of enhanced spiritual wellbeing” |
vs. Medical Diagnoses
Medical diagnoses name the disease at hand, its pathology, and does not describe human responses. As long as the disease remains, this diagnosis does not change. In contrast, nursing diagnoses describe human responses to the disease process or health problem. These change throughout the disease process and can change frequently.
Components of a Nursing Diagnosis
- Problem: the health problem, response, or status of the patient. These are paired with qualifiers that add context to the problem. These are words such as “Deteriorated”, “Vulnerable to threat”, “Incomplete”. These are diagnostic labels that direct the formation of client goals and desired outcomes.
- Etiology: one or more probably causes of the health problem, giving direction to required nursing therapy. These specify the health problem to the individual at hand, providing client-centered care.
- Signs and Symptoms: clusters of signs and symptoms that indicate the presence of a particular diagnostic label. These are used for actual nursing diagnoses, and are not available for risk nursing diagnoses.
Diagnostic Process
- Analyze Data: collect and compare significant assessment cues against standards. Cluster these cues for a tentative hypothesis, and identify gaps and inconsistencies (conflicting or erroneous data).
- Identify Health Problems, Risks, or Strengths
- Formulate Diagnostic Statement: using the components of the nursing diagnosis to create a one-part, two-part, or three-part diagnosis:
- One-part Statement: only the problem (nursing diagnosis) is stated, with no etiology or signs/symptoms necessary. Ex.: “Readiness for enhanced community coping”.
- Two-part Statement: the problem and its etiology, often used for risk statements, as patients do not yet have signs and symptoms. Ex.: “Non-adherence (diabetic diet) related to denial of having disease”, “Anxiety related to threat to physiologic integrity: possible cancer diagnosis”
- Three-part Statement: a full statement of the three components of a nursing diagnosis. Ex.: “Impaired self-esteem related to feelings of rejection by husband as manifested by hypersensitivity to criticism; states “I don’t know if I can manage by myself” and rejects positive feedback”.
Writing a Nursing Diagnosis
- State a problem, not a need:
Alteration in fluidrather thanFluid replacement. - Word the statement so that it is legally advisable; avoid “incriminatory” statements that predispose the nurse to complaints:
Altered skin integrity related to improper positioninginsinuates that the problem is caused by negligent care →Altered skin integrity related to immobility - Use non-judgmental statements:
Impaired spirituality related to inability to attend church services secondary to immobilityrather thanImpaired spirituality related to strict rules necessitating church attendance. - Avoid redundancy between the problem and etiology:
Altered skin integrity related to ulceration of sacral areais a self-referencing diagnosis. Instead, writePotential for altered skin integrity related to immobility. - Ensure correctness of the cause-and-effect relationship:
Pain related to headacheis invalid as the headache does not cause pain; it is pain itself. Instead,Pain: severe headache related to avoidance of narcotics due to fear of addictionprovides an appropriate etiological statement. - Word the diagnosis specifically and precisely:
Alteration in mucous membrane integrity related to noxious agentidentifies the etiology, but does not specify the type of interventions potentially required. Instead,Alteration in mucous membrane integrity related to decreased salivation secondary to radiation of neckcan point nurses to the proper interventions to use. - Use nursing terminology rather than medical terminology to describe the client’s response:
Potential for pneumoniais medical in nature;Potential for altered respiratory status related to accumulation of secretions in lungsbetter fits a nurse’s field of knowledge. Similarly, etiologies should also use nursing terminology:...related to accumulation of secretion in lungsrather than...related to pneumonia.
List of the accepted nursing diagnoses for use and research (NANDA Diagnoses, Prioritized Interventions, and Rationales 16th Ed., 2021 - 2023)
Diagnosis Modifiers Activity Planning Ineffective, Risk for Ineffective Activity Tolerance Decreased Acute Substance Withdrawal Syndrome Risk for Adverse Reaction to Iodinated Contrast Media Risk for Airway Clearance Ineffective Allergy Reaction Risk for Anxiety [specify level], Death Aspiration Risk for Attachment Risk for Impaired Autonomic Dysreflexia (As one-part diagnosis), Risk for Behavior Disorganized Infant, Readiness for Enhanced Disorganized Infant Bleeding Risk for Blood Glucose Level Risk for Unstable Body Image Disturbed Breast Milk Production Insufficient Breastfeeding Ineffective, Interrupted, Readiness for Enhanced Breathing Pattern Ineffective Cardiac Output Decreased, Risk for Decreased Cardiovascular Function Risk for Impaired Childbearing Process Readiness for Enhanced, Risk for Ineffective Chronic Pain Syndrome - Comfort Impaired, Readiness for Enhanced Communication Impaired Verbal, Readiness for Enhanced Confusion Acute, Chronic, Risk for Acute Constipation (As one-part diagnosis), Chronic Functional, Perceived, Risk for, Risk for Chronic Functional Contamination (As one-part diagnosis), Risk for Continence Impaired Bowel Coping Compromised Family, Defensive, Disabled Family, Ineffective, Ineffective Community, Readiness for Enhanced, Readiness for Enhanced Community, Readiness for Enhanced Family Decision-Making Readiness for Enhanced Decisional Conflict (As one-part diagnosis) Denial Ineffective Dentition Impaired Development Delayed Child, Risk for Delayed Child Diarrhea (As one-part diagnosis) Disuse Syndrome Risk for Disturbed Family Identity Syndrome (As one-part diagnosis), Risk for Diversional Activity Engagement Risk for Decreased Dry Eye Risk for Dry Eye Self-Management Ineffective Dry Mouth Risk for Eating Dynamics Ineffective Adolescent, Ineffective Child, Ineffective Infant Electrolyte Imbalance Risk for Elimination Impaired Urinary Elopement Attempt Risk for Emancipated Decision-Making Impaired, Readiness for Enhanced, Risk for Impaired Emotional Control Labile Energy Field Imbalanced Exercise Engagement Readiness for Enhanced Falls Risk for Adult, Risk for Child Family Processes Dysfunctional, Interrupted, Readiness for Enhanced Fatigue (As one-part diagnosis) Fear (As one-part diagnosis) Female Genital Mutilation Risk for Fluid Volume Deficient (Hyper-/hypotonic), Deficient (Isotonic), Excess, Risk for Deficient, Risk for Imbalanced Frail Elderly Syndrome (As one-part diagnosis), Risk For Gas Exchange Impaired Gastrointestinal Motility Dysfunctional, Risk for Dysfunctional Grieving Readiness for Enhanced, Maladaptive, Risk for Maladaptive Growth Risk for Disproportionate Health Deficient Community Health Behavior Risk-prone Health Literacy Readiness for Enhanced Health Maintenance Behaviors Ineffective Health Self-Management Ineffective, Ineffective Family, Readiness for Enhanced Home Maintenance Behaviors Ineffective, Readiness for Enhanced, Risk for Ineffective Hope Readiness for Enhanced Hopelessness (As one-part diagnosis) Human Dignity Risk for Compromised Hyperbilirubinemia Neonatal, Risk for Neonatal Hyperthermia (As one-part diagnosis) Hypothermia (As one-part diagnosis), Neonatal, Risk for, Risk for Neonatal, Risk for Perioperative Immigration Transition Risk for Complicated Impulse Control Ineffective Incontinence Disability-Associated Urinary, Mixed Urinary, Stress Urinary, Risk for Urge Urinary, Urge Urinery Infection Risk for Injury Risk for, Risk for Urinary Tract Insomnia (As one-part diagnosis) Knowledge Deficient, Readiness for Enhanced Latex Allergy Reaction Risk for Lifestyle Sedentary Liver Function Risk for Impaired Loneliness Risk for Lymphedema Self-Management Ineffective, Risk for Ineffective Maternal-Fetal Dyad Risk for Disturbed Memory Impaired Metabolic Imbalance Syndrome Risk for Mobility Impaired Bed, Impaired Physical, Impaired Wheelchair Mood regulation Impaired Moral Distress (As one-part diagnosis) Motor Development Delayed Infant Mucous Membrane Integrity Impaired Oral Mucous Membrane Risk for Impaired Oral Nausea (As one-part diagnosis) Neonatal Abstinence Syndrome (As one-part diagnosis) Neurovascular Dysfunction Risk for Peripheral Nipple-Areolar Complex Injury (As one-part diagnosis), Risk for Nutrition Less than Body Requirements, Imbalanced, Readiness for Enhanced Obesity (As one-part diagnosis) Occupational Injury Risk for Overweight (As one-part diagnosis), Risk for Pain Acute, Chronic, Labor Parenting Impaired, Readiness for Enhanced, Risk for Impaired Perioperative Positioning Injury Risk for Personal Identity Disturbed, Risk for Disturbed Poisoning Risk for Post-Trauma Syndrome (As one-part diagnosis), Risk for Power Readiness for Enhanced Powerlessness (As one-part diagnosis), Risk For Pressure Injury Adult, Risk for Adult, Child, Risk for Child, Neonate, Risk for Neonate Protection Ineffective Rape-Trauma Syndrome (As one-part diagnosis) Relationship Ineffective, Readiness for Enhanced, Risk for Ineffective Religiosity Impaired, Readiness for Enhanced, Risk for Impaired Relocation Stress Syndrome (As one-part diagnosis), Risk for Resilience Impaired, Readiness for Enhanced, Risk for Impaired Retention Acute Urinary, Chronic Urinary, Risk for Urinary Role Conflict Parental Role Performance Ineffective Role Strain Caregiver, Risk for Caregiver Self-Care Readiness for Enhanced Self-Care Deficit Bathing, Dressing, Feeding, Toileting Self-Esteem Chronic Low, Risk for Chronic Low, Risk for Situational Low, Situational Low Self-Mutilation (As one-part diagnosis), Risk for Self-Neglect (As one-part diagnosis) Sensory Perception Disturbed Auditory, Disturbed Gustatory, Disturbed Kinesthetic, Disturbed Olfactory, Disturbed Tactile, Disturbed Visual Sexual Dysfunction (As one-part diagnosis) Sexuality Pattern Ineffective Shock Risk for Sitting Impaired Skin Integrity Impaired, Risk for Impaired Sleep Readiness for Enhanced Sleep Deprivation (As one-part diagnosis) Sleep Pattern Disturbed Social Interaction Impaired Social Isolation (As one-part diagnosis) Sorrow Chronic Spiritual Distress (As one-part diagnosis), Risk For Spiritual Well-Being Readiness for Enhanced Standing Impaired Stress Overload (As one-part diagnosis) Suck-Swallow Response Ineffective Infant Sudden Infant Death Risk for Suffocation Risk for Suicidal Behavior Risk for Surgical Recovery Delayed, Risk for Delayed Surgical Site Infection Risk for Swallowing Impaired Thermal Injury Risk for Thermoregulation Ineffective, Risk for Ineffective Thought Process Disturbed Thromosis Risk for Tissue Integrity Impaired, Risk for Impaired Tissue Perfusion Ineffective Peripheral, Risk for Decreased Cardiac, Risk for Ineffective Cerebral, Risk for Ineffective Peripheral Transfer Ability Impaired Trauma Risk for Physical, Risk for Vascular Unilateral Neglect (As one-part diagnosis) Ventilation Impaired Spontaneous Ventilatory Weaning Response Dysfunctional, Dysfunctional Adult Violence Risk for Other-Directed, Risk for Self-Directed Walking Impaired Wandering Sporadic, Continuous
Planning
Planning involves designing nursing activities. It is required to prevent, reduce, or eliminate a client’s health problems through an intentional, systematic process of decision-making and problem-solving. It utilizes the client’s assessment data and diagnostic statements for direction in formulating client goals and designing nursing interventions.
Nursing Care Plan
The end product of this phase is a Nursing Care Plan (NCP). NCPs may be standardized (used for specific populations with predictable, common problems) and/or individualized (tailored to unique needs).
| Type of Planning | Description |
|---|---|
| Initial Planning | Admission assessment that develops the initial comprehensive plan of care that is initiated as soon as possible. |
| Ongoing Planning | Occurs at the beginning of every shift for determining required care for a nurse’s shift. It determines: - Changes in health status - Set priorities and decide problems to focus on - Coordinate the nurse’s activities |
| Discharge Planning | The anticipation and planning for client needs after discharge. Effective discharge planning begins at first client contact. |
Creating NCPs
An NCP should contain aspects of restoration of health, prevention of disease, and maintenance of health. On-going assessment is also outlined for continual use of the care plan.
- Date and sign the plan. This is done for evaluation, review, and future planning. Accountability is expressed with a signature.
- Category headings are used to compartmentalize the pertinent entries for each phase of the nursing process.
- Use standardized, approved medical notation. This keeps the plan succinct yet meaningful between members of the healthcare team.
- Nurses may refer to procedure books rather than outline procedures within the plan itself, e.g., “See unit procedure book for tracheostomy care.”
- Be specific. The details of an intervention (e.g., duration, time) is outlined comprehensively to assure proper compliance between shifts.
- Individualize. Care is not always a stenciled activity. Client choices and preferences are considered when planning care.
- Multidisciplinary Coverage: collaborative interventions should be used, adhering to the holistic aspect of care. Referrals to dietitians, occupational therapists, physicians, etc. are included in the care plan.
- Discharge Planning: plans for discharge and home care needs should be included in the care plan.
Planning Process
- Priority Setting: the assignment of problems as high, medium, or low priority.
| Priority Level | Cases, Examples |
|---|---|
| High | Life-threatening; impaired cardiopulmonary function - Altered respiratory status (r/t secretions, pain, fatigue) - Alteration in fluid volume (fluid loss r/t fever, diaphoresis) |
| Medium | Health-threatening; acute illness and decreased coping ability - Anxiety (r/t difficulty breathing) - Concerns over work and parenting roles |
| Low | Normal developmental needs; requires minimal nursing support - Impaired nutritional status (r/t anorexia, nausea, increased metabolism) - Self-care deficit (r/t weakness) |
- Establishing Client Goals/Desired Outcomes: goals are broad statements, while desired outcomes are specific, measurable statements. Here are some examples:
| Diagnosis | Goal | Desired Outcomes |
|---|---|---|
| Alteration in mobility | - Improved mobility - Ability to bear weight on affected leg | - Ambulate with crutches by the end of the week - Stand without assistance by the end of the month |
| Altered respiratory status related to poor cough effort, secondary to incision pain and fear of damaging sutures | - Effective airway clearance | - Clear lungs upon auscultation during the entire postoperative period. - No skin pallor or cyanosis by 12 hours postoperation. - Demonstrate good cough effort within 24 hours postoperation. |
Timespan
Goals can be generally considered as short-term (within days or even hours), or long-term (within weeks or months).
- Selecting Nursing Interventions:
- Independent interventions are those activities which nurses are able to initiate on the basis of their knowledge and skills.
- Dependent interventions are those carried out under the orders of a licensed physician.
- Collaborative interventions are actions the nurse carries out with other health team members, such as physical therapists, social workers, and dietitians.
- Writing Individualized Nursing Interventions: written interventions follow the verb-condition/modifier-time element format. For example:
- Measure and record (verb) ankle circumference (condition/modifier) daily at 0900 (time element)
- Apply (verb) spiral bandage firmly (condition/modifier) to left lower leg.
- Assist (verb) client with tub bath (condition/modifier) daily at 0700 (time element)
Delegation
The planned care may be delegated to those qualified, with supervision. It is the task of the delegator to determine the most appropriate and qualified delegees for the task. Certified nursing assistants (CNAs) and unlicensed assistive personnel (UAPs) are generally allowed to aid in positioning, feeding, recording of intake and output, ambulating, and vital signs (but not interpretation) and bathing. The following are never delegated:
- Unstable clients: newly admitted patients, those returning from procedures, those post-operative, those with unstable vital signs, unstable blood sugar, and unstable neurological status
- Evaluation: interpreting data, lab values, pain, and vital signs are all tasks of the nurse
- Assessment: initial, first, primary assessment of the patient
- Teaching: initial, first, primary education of the patient
Implementation
The action phase in which the nurse performs nursing interventions. The client is reassessed to make sure the interventions are still valid, then care is provided. Requisite assistance is obtained for the procedure. During provision, supervision is imperative for delegated care. All nursing activities are documented.
- Reassessing the client is done prior to care to determine if intervention is still required. This applies to independent and dependent actions, and the nurse exerts their clinical judgment as necessary.
- Determining the need for assistance is done to perform care best provided collaboratively. This enhances safety and efficiency, especially in the case of a nurse who is not yet experienced in practice.
- Supervising delegated or assigned care is a legal and ethical obligation under the doctrine of respondeat superior. All care activities must be implemented according to the care plan.
Respondeat Superior is a doctrine of law to "let the principal be held responsible", extending the liability of subordinates to their superiors.
- Documenting Nursing Activities: completion of the implementation phase occurs after recording the interventions and client responses in the nursing progress notes. This is done immediately after implementation, and never in advance.
Good Characteristics of Nursing Interventions
- Adaptable: care is individualized to patient health status, beliefs, environment, etc.
- Based on professional standards: scientifically rational, with proper considerations and education on side effects and complications to watch out for.
- Clear and understandable; any questionable interventions are clarified and revised if erroneous.
- Dignified. The client’s self-esteem is preserved as much as possible.
- Encouraging for the patient, especially in exercising independence, control, and active participation in their care.
- Holistic. It should be safe and applied with teaching, support, and comfort.
Evaluation
The final phase of the nursing process. Conclusions are drawn whether or not the nursing interventions should be terminated, continued, or changed. There are five components of evaluation:
| Component | Question |
|---|---|
| Collecting Data | Has the client’s condition improved or deteriorated since the last evaluation? |
| Comparing Data | What improvements have been made in client care? |
| Relating Nursing Activities | Were the nursing interventions able to attain the planned outcomes? |
| Drawing Conclusions | Which outcomes have been attained? |
| Continuation, Modification, or Termination | Are there any changes necessary in the plan of care to attain the desired outcomes? |
- Collecting Data: assessment of the client for the effects of implemented care. This follows the same principles as applied in the Assessment phase.
- Comparing Data: the re-assessment is compared to the data for desired outcomes. This is generally divided into three phrases in documentation: Goal met, Goal partially met (i.e., not all desired outcomes were reached), and Goal not met. These are followed by the assessment data supporting such a declaration.
- Relating Nursing Activities: the interventions are correlated to the outcomes to determine their role in reaching goals. This determines if interventions are necessary, appropriate, effective, or efficient.
- Drawing Conclusions: the previous steps compile into this final output. It concludes whether interventions should be continued, revised, or discontinued:
| Status | Further Action |
|---|---|
| Goal Met: the problem has been resolved and its risk factors are no longer present | Care is discontinued |
| Goal Met: the problem has been resolved but its risk factors remain present | The care plan is kept for use when necessary. |
| Goal Partially Met: the problem remains, but some goals have been met | Continue nursing intervention, consider revisions |
| Goal Partially Met or Goal Not Met | The care plan may need to be revised, or has not yet been able to exert its full effect. |
Agency SOP
Agencies have differing standards for NCP modifications. In some, modifications may be made via strikethrough (
like this) for the care plan, highlighting, or indicating revisions as appropriate for electronic charting systems. Writing “Discontinued”, “Goal Met”, or “Problem Resolved” may also be appropriate.
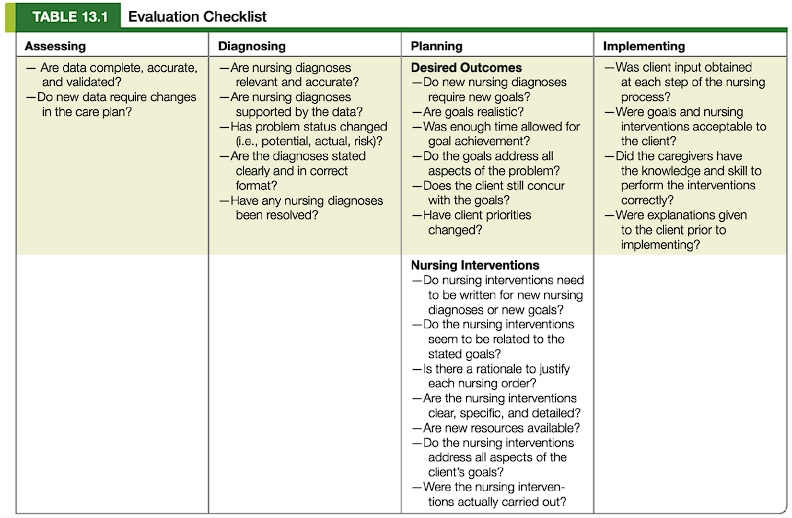
Evaluation Checklist
Below is a simple guideline for evaluating whether the stages of the nursing process were performed adequately: