Digestive System
The digestive system consists of a long tube also known as the alimentary canal where ingested substances travel and undergo mechanical and chemical digestion for conversion into absorbable units of food for nutrition. In conjunction with this canal, accessory organs of digestion (liver, gallbladder, salivary glands, pancreas) aid in the digestion of food.
GIT Subdivisions and Function
The Upper GIT, starting from the mouth to the small intestine, is where digestion primarily takes place.
The Lower GIT, starting from the large intestine to the anus, involves:
- Absorption; the reabsorption of water that converts stool into its formed, solid state.
- Synthesis of Vitamin K by the normal gut flora E. coli, which makes up roughly 50% of an individual’s Vitamin K. This is necessary for the production of clotting factors X, IX, VII, and II (Vitamin K dependent clotting factors). This is the mechanism behind the importance of Vitamin K in stopping bleeding.
- Putrefaction also occurs, where E. coli interacts with fecal materials to produce flatus, a combination of carbon dioxide, carbon monoxide, methane, and ammonia
GI Bleeding
Gastrointestinal bleeding can occur along any part of the alimentary canal. In general, this is also divided between Upper GI Bleeding (UGIB) and Lower GI Bleeding (LGIB), which present differently:
- UGIB gives time for the blood to be acted upon by digestive enzymes and the acids of the body. This converts its color into a dark, tarry form that produces melenic stool (melena); stool that is dark, tarry, and foul-smelling, one characteristic of upper GI bleeding.
- LGIB occurs in the non-digestive part of the alimentary canal, which allows blood to retain its original color upon being excreted along with stool. This appears as hematochezia; stool that is red and bloody.
Abdominal Assessment
Compared to the normal sequence of assessment (IPPA), abdominal assessment follows IAPePa: inspection, auscultation, percussion, and palpation. This sequence prioritizes auscultation as percussion and palpation can alter bowel sounds when performed, modifying assessment findings.
- Inspection: view the skin for its color, common discoloration signs (Grey-Turner, Cullen’s), masses, distention, and contour
- Auscultation: listening for bowel sounds in all quadrants for one full minute, normally occurring from 5 to 35 sounds in 60 seconds. Bowel sounds often change in conditions that involve abdominal cramping, diarrhea, or obstructions.
- Percussion
- Palpation
The abdominal areas may be subdivided into four quadrants or nine regions:
- Nine-Region System: this system divides the abdomen into nine areas using two horizontal and two vertical lines (midclavicular lines). The lowest region ends at the level of the highest part of the pelvic bone (transtubercular line), and the highest region ends at the end of the ribcage (subcostal line).
| Left | Middle | Right |
|---|---|---|
| Left Hypochondriac | Epigastric | Right Hypochondriac |
| Left Lumbar | Umbilical | Right Lumbar |
| Left Iliac (Inguinal) | Hypogastric (Suprapubic) | Right Iliac (Inguinal) |
- Four-Quadrant System: this system divides the abdomen into four with the midline from the xiphoid to the symphysis pubis, and a transverse cut across the umbilicus.
Nausea and Vomiting
The part of the brain that produces vomiting when stimulated is the chemoreceptor trigger zone (CTZ). Any stimulation of this zone results in vomiting. Some of these stimuli include:
- Any inflammation in the abdominal region
- Any obstruction in the abdominal region
- Increased intracranial pressure
- Vertigo or dizziness
- Anticancer drugs
- Early pregnancy
- Sensory exposure to gross or noxious elements
Inflammatory Disorders
Inflammatory diseases share common presentations, and are those disorders that end in “-itis”. The primary manifestations of inflammatory disorders include (a) pain, (b) nausea and vomiting, and (c) indigestion (dyspepsia).
- Gastritis
- Peptic Ulcer Disease (PUD); A.K.A. Erosive Inflammation
- Inflammatory Bowel Diseases (IBD):
- Regional Enteritis; A.K.A. Chron’s Disease
- Ulcerative Colitis
- Appendicitis
- Diverticulitis
- Cholecystitis
- Pancreatitis
Pain Location & Associated Disorders
Location Disorders LUQ Pancreatitis LLQ Ulcerative colitis, Diverticulitis RUQ Cholecystitis RLQ Crohn’s Disease, Appendicitis Epigastric Region Gastritis, Peptic Ulcer Disease
Non-inflammatory Disorders
Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome is a functional (no causative structural defects) disorder with an unknown cause— an idiopathic disorder. However, this has been theorized to be caused by neural or hormonal defects in gastrointestinal regulation.
- Risk Factors: stress, family history
- Signs and Symptoms: IBS is classified as IBS-c (results in constipation), IBS-d (results in mucoid diarrhea), or IBS-m/IBS-a (results in mixed or alternating diarrhea and constipation). Additionally the following also occur:
- Indigestion (dyspepsia)
- Abdominal pain
- Diagnostic Evaluation: mainly exclusionary, as there is no test specific to IBS. These include colonoscopy, CBC, ESR (elevated in inflammation), imaging (UTZ)
- Management is palliative; symptom-based:
- Diarrhea: high protein (prevent fluid shifting), low residue, high fiber and fluid diet with fluid replacement (Oresol). In severe cases, antidiarrheals (Loperamide) may be given.
- Constipation: low fat, high fiber diet with increased fluid intake. In severe cases, laxatives may be prescribed.
- Control symptoms and exacerbations: low residue, high fiber diet.
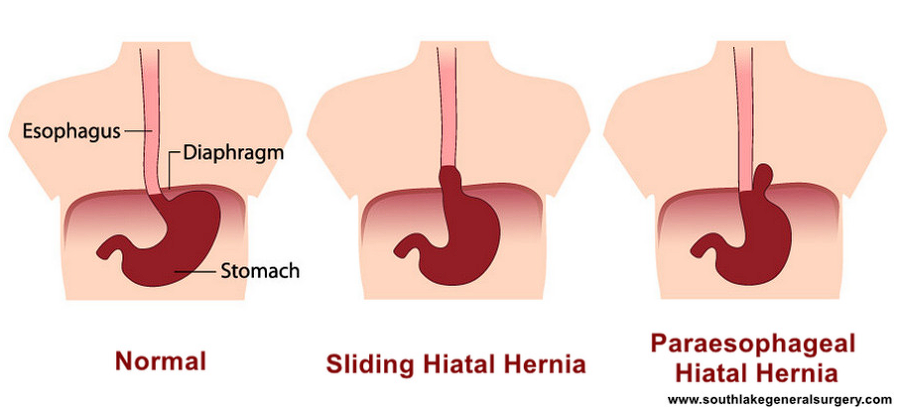
Hiatal Hernia
The protrusion of the stomach upwards through the diaphragmatic hiatus. This hiatus is part of the muscle that divides the thoracic cavity and the peritoneal cavity. The hiatus is the point where the esophagus connects to the stomach. This may be congenital or acquired— increased intraabdominal pressure, such as in obesity, pregnancy, and lifting.
- Types:
- Sliding Hernia: the herniation progresses towards the esophagus
- Rolling (Paraesophageal) Hernia: the herniation progresses sidewards
- Mixed-Type Hernia (combination of both)
- Signs and Symptoms: the most prominent clinical manifestation of a hiatal hernia is pyrosis (heartburn) resulting from the compromised lower esophageal sphincter and the heightened intraabdominal pressure. As such, this hernia is one of the etiologies of GERD.
- Esophagitis, dysphagia (difficult), and odynophagia (pain) are all caused by irritation and injury to the esophageal tract by gastric acid.
- Chronic irritation of the esophageal epithelium causes its normally squamous cells to undergo metaplasia into columnar cells, which is known as Barrett’s Esophagus— the most common precancerous condition of the esophagus.
- Nursing Diagnosis: Pain
- Diagnostic Evaluation: (a) esophagoscopy and (b) barium swallow with imaging.
- Management: the main goal is to prevent reflux:
- Keep the patient upright 1 to 2 hours after eating; do not lie down.
- No bedtime snacks
- Elevate the head of bed by 6 inches to reduce nighttime reflux.
- Avoid food and drug that can decrease the lower esophageal sphincter’s ability to constrict: soft drinks, alcohol, fatty foods, chocolate, spices/spiciness, Fosamax, Valium
- Avoid activities that increase intraabdominal pressure: lifting, straining, Valsalva maneuver, bending by the stomach
- Avoid constrictive clothing
- Use antacids 30 to 60 minutes after eating
- Use histamine receptor blockers (H₂ antagonists) such as Ranitidine to decrease acid production
- The most effective drugs for GERD are proton pump inhibitors (Omeprazole, Esomeprazole) to decreased acid production.
- Surgery is the last consideration.
Inguinal and Femoral Hernia
- An inguinal hernia is the protrusion of a loop of intestine through the inguinal canal due to weakness or defect in the abdominal muscle.
- A femoral hernia is the protrusion of a loop of intestine through the femoral canal where the femoral artery and vein also pass through.
These hernias run the risk of strangulation where the loop of intestine is constricted and potentially injured. In such a case, herniorrhaphy becomes emergent. Otherwise, surgical correction may be considered as an elective surgery.
Liver Cirrhosis
Liver Cirrhosis is an irreversible, progressive scarring (fibrosis) of the liver. This is commonly caused by alcohol (Laennec’s Cirrhosis), infection (hepatitis), drugs (hepatotoxicity), hepatoma (Liver Cancer), and idiopathy (biliary cirrhosis). Specifically for infection and hepatotoxicity, they are considered as post-necrotic cirrhosis.
| Signs of Liver Dysfunction | Pathophysiology |
|---|---|
| Jaundice, Decreased Fat Absorption | Emulsification of fats by bile is required for absorption. The liver produces bile out of water, bilirubin, cholesterol, and bile salts. In liver dysfunction, bilirubin is not taken up by the liver and jaundice occurs as bilirubin levels increase. Decreased bile production results in decreased fat absorption. |
| Weight Loss, Weakness | The liver is the site of fat metabolism— lipogenesis, lipolysis, and gluconeogenesis. In liver dysfunction, weight loss and weakness occur as fat is no longer stored or used in the body as energy. |
| Fatigue | Glycogenesis and glycogenolysis as processes in carbohydrate metabolism in the liver become impaired, which results in easy fatigability from decreased energy stores (glycogen). |
| Bipedal Edema | Albumin, the major protein in the blood, is produced in the liver. It maintains intravascular pressure by exerting oncotic (attractive) pressure to fluids, maintaining circulating volume. When albumin decreases in liver dysfunction, oncotic pressure decreases, and fluid leaves the intravascular space, producing edema (bipedal). |
| Hepatic Encephalopathy | Protein metabolism produces ammonia, which the liver converts into urea, which can be excreted by the urine. If it is unable to do so, ammonia levels rise, which result in hepatic encephalopathy, a severe complication of liver cirrhosis. |
| Carbohydrate Metabolism | |
| Vitamin Deficiency | Fat-soluble vitamins are absorbed along with fats, which rely on emulsification by bile. If bile is insufficient, the fat-soluble vitamins (ADEK) may become deficient as the body fails to absorb them. Additionally, some B vitamins are also stored in the liver. |
| Bleeding | All clotting factors are produced by the liver. In liver dysfunction, the patient becomes prone to bleeding problems. |
| Altered Pharmacokinetics | Biotransformation of drugs i.e. the metabolism of drugs into inactive metabolites for excretion is primarily done by the liver. In liver dysfunction, these patients experience altered pharmacokinetics and normal doses of drugs may cause toxic effects. |
| Signs of Portal Hypertension | Pathophysiology |
|---|---|
| Normal physiology of the portal vein → | All the blood returning from the gastrointestinal tract passes through the portal vein. This blood contains food and drugs and are immediately metabolized in the liver before entering circulation through the hepatic vein then to the inferior vena cava. |
| Ascites | Tissue scarring stiffens the liver, increasing pressure in the portal vein. It is in portal hypertension that fluid escapes the intravascular compartment into the peritoneum— ascites. |
| Neovascularization— Hemorrhoids, Esophageal Varices | This also causes blood to back up in gastrointestinal circulation, resulting in hemorrhoids (recto-anal varices) and esophageal varices, which are fragile and easily rupture; bleeding risks. Combined with impaired production of clotting factors, patients are highly susceptible to hemorrhage. |
| Vascular Changes— Caput Medusae, Spider Angiomas | Blood from GI circulation escapes through collateral vessels due to portal hypertension, forming prominent distended abdominal veins (caput medusae) and spider angiomas (pathognomonic of liver cirrhosis) |
- Diagnostic Examination: the most definitive test for liver cirrhosis is a liver biopsy. In a liver biopsy, the patient is positioned supine with a pillow under the right upper quadrant. After the procedure, a common complication is bleeding, hence the patient must be positioned right side-lying with a pillow under the right upper quadrant. This compresses the biopsy site, reducing bleeding.
- Additionally, elevated liver enzymes (AST, ALT) can show a result of up to three times normal value.
- Imaging: Ultrasound, MRI, CT Scan
- Early Stage Management: non-specific symptoms— weight loss, weakness, fatigue, bipedal edema (altered metabolism, albumin production). Nursing Diagnoses: Fluid Volume Excess, Imbalanced Nutrition, Less Than Body Requirements, Fatigue, Activity Tolerance, Risk for Injury:
- Restrict fluids and sodium or use diuretics (potassium-sparing) as ordered.
- Diet: low sodium, low fat, low cholesterol, high iron (for anemia), high albumin
- Monitor intake and output, vital signs, and weigh the patient daily
- Provide rest periods, and ensure safety (for weakness and fatigue)
- Slow down the progression of the disease: avoid alcohol, follow diet regimen, avoid fatigue, stress, infection, hepatotoxic drugs, and other precipitating factors.
- Late Stage Management: specific symptoms also appear in addition to early signs— ascites, dyspnea, anorexia, jaundice, portal hypertension (hepatomegaly, esophageal varices, rectoanal varices, hemorrhoids, bleeding), vascular changes (caput medusae, spider angioma), and complications (hepatic encephalopathy, primary peritonitis, hepatorenal syndrome)
- As earlier, continue restrictions (Fluid, Na) and monitoring (I&O, VS, Wt). However, protein is now limited, as this may contribute to hepatic encephalopathy.
- Rest and safety is still required. Importantly, avoid bleeding:
- Avoid trauma, avoid variceal rupturing (straining, coughing)
- Use an electric, soft-bristled toothbrush
- The use of a Sengstaken-Blakemore Tube, a three-lumen tube, can apply physical support to esophageal varices with a balloon (second lumen) while maintaining patency with the stomach (first lumen), and anchoring the tube in place (third lumen). While in place, watch out for airway problems due to its proximity to the trachea. In case of anchor rupture, the pressure of the second lumen pushes the tube upwards and obstructs breathing. The nurse needs to rupture the tube with a pair of scissors and remove the tube.
- Blood transfusion: PRBC may be required if bleeding is severe. FFP and Cryoprecipitate may be given to restore clotting factors.
- Diet: restrict sodium, low protein, low fat, low cholesterol, high iron (for anemia), high vitamin content (ADEK/B). Restrict alcohol.
- Position the patient on reverse Trendelenburg to localize ascites away from the diaphragm to relieve breathing.
- Paracentesis may be used if ascites is severe. Patients empty the bladder and are positioned upright (sitting). A catheter is anchored to just below the umbilicus to serve as an exit point. Not all fluid is removed at once to avoid causing hypotension.
- Skin care may be required for pruritic jaundice.
- Beta-blockers may be used to reduce portal hypertension.
- Manage complications:
- Primary peritonitis, treated with massive doses of antibiotics
- Hepatorenal syndrome: kidney injury
- Hepatic encephalopathy: a metabolic brain disease characterized by increased ammonia in the blood causing an altered level of consciousness. There are staging classifications:
- Stage I: Confusion, asterixis (flapping tremor)
- Stage II: Lethargy, asterixis
- Stage III: Stuporous, potential loss of asterixis
- Stage IV: Comatose, no asterixis present
- Controlling hepatic encephalopathy: restrict protein in the diet, avoid bleeding (hemolysis eventually produces ammonia), decrease putrefaction that contributes to ammonia formation (remove fecal materials with laxatives/enema or remove gut bacteria with antibiotics)
- Maintain privacy, prevent immobility complications, promote safety, and continue communicating with the patient, even if comatose.
Sample Questions
Gastrointestinal System
Which of the following instructions in inappropriate for a nurse to give to a patient who has gastroesophageal reflux disease?
- Take prescribed antacids before eating
- Place blocks under the legs of the head of the bed
- Eating a high-fat, low-protein must be avoided
- Do not lie down for one hour after eating
Rationalization
A nurse would assess a patient who has undergone a total gastrectomy for late symptoms of dumping syndrome, which include:
- Diaphoresis, lightheadedness
- Facial flushing, paresthesia
- Disorientation, vomiting
- Diarrhea, hypotension
Rationalization
Which of the following statements, if made by a patient who has diverticulosis, would indicate to the nurse that the patient is following the diet plan correct?
- I eat meat five times a week
- I do not eat fried foods
- I drink water instead of coffee
- I eat macaroni salad every day
Rationalization
A nurse should expect a Sengstaken-Blakemore tube to be ordered for a patient who has bleeding esophageal varices in order to apply direct pressure and
- Cause vasoconstriction of the splenic artery
- Ensure airway patency
- Provide for enteral nutrition
- Stop bleeding
Rationalization
A client with cholecystitis is being assessed for Murphy’s sign. The nurse is correct when they notice:
- The client stops breathing in when pressure is applied to the RUQ
- The client stops breathing out when pressure is applied to the RUQ
- The client stops breathing in when pressure is applied to the LUQ
- The client stops breathing out when pressure is applied to the LUQ
Rationalization
A client with liver cirrhosis manifests asterixis, jaundice, and anorexia due to
- Liver dysfunction
- Portal hypertension
- Both conditions
- Neither of these
Rationalization
A client with acute pancreatitis complains of severe pain, which of the following independent nursing intervention is a priority?
- Narcotics as ordered
- Position the client comfortably
- Place the client on NPO
- All of the above
Rationalization
The nurse would expect which of these assessment findings in a client with gastric ulcers?
- Pain occurring at night
- Pain relieved by eating
- Gnawing epigastric pain
- All of the above
Rationalization
The client who has underwent a Billroth I procedure is taught that the procedure involves:
- Removal of the stomach and anastomosing the stump to the duodenum
- Removal of the stomach and duodenum and anastomosing the stump to the jejunum
- Bypassing the stomach and connecting it to the ileum
- Removal of the duodenum and anadstomosing the stomach to the jejunum
Rationalization
In caring for a client with hiatal hernia, which of the following should not be included in a teaching plan regarding the causes?
- To avoid heavy lifting
- A dietary plan avoiding soda
- Its prevalence on obese persons
- Its prevalence on women
Rationalization
The most fatal complication of Choledocholithiasis is ascending cholangitis which may complicate to develop shock, the initial manifestation of which includes the following except?
- Jaundice
- HR 120/min
- Hyperventilation
- No exception
Rationalization
A client with liver cirrhosis has severe ascites and being prepared for paracentesis, prior to the procedure the client is asked to:
- Prepare for paracentesis
- Empty the bladder
- Place the client in a reverse Trendelenburg position
- All of the above
Rationalization
After pyloroplasty, which of the following interventions promote rapid gastric emptying?
- Simple sugar in the diet
- Moderate fat intake
- Liquid must be taken in between meals
- Upright position after meals
Rationalization
A client with possible appendicitis is being assessed, which of the following is a sign of complication?
- Severe vomiting
- High grade fever
- WBC 15,000
- Rigid, board-like abdomen
Rationalization
The I in IBD stands for
- Irritable
- Inflammatory
- Infectious
- Incredible
Rationalization
A clinic nurse is providing health teaching for a patient newly diagnosed with gastroesophageal reflux disease. Which of the following needs no further teaching for the patient?
- Change of dietary pattern to small frequent feedings and bedtime snack
- Avoiding wearing of tight socks
- Use of magnesium carbonate (Gaviscon) to decrease acid production
- Avoidance of bending, stooping, or slumping posture
Rationalization
Postoperatively, the patient develops dumping syndrome. Which of the following statements, if made by the patient, should indicate to the nurse that furhter dietary teaching is unnecessary?
- “I should eat bread with each meal.”
- “I should eat meals more frequently.”
- “I should lie down after eating.”
- “I should drink fluids with my meals.”
Rationalization
A client with peptic ulcer disease would be given the following medications, except:
- Antacid
- Ranitidine
- Metronidazole
- No exception
Rationalization
Which of the following would predispose the client to the development of chronic pancreatitis?
- Cystic fibrosis
- Alcoholism
- Fatty foods
- All of the above
Rationalization
A client being treated for esophageal varices has a Sengstaken-Blakemore tube inserted to control the bleeding. The most important assessment for the nurse is to check:
- The ability to swallow
- IV fluids for the shift
- A patent airway
- Check that the balloon is deflated on a regular basis
Rationalization
The nurse notes that there is documentation of the presence of asterixis. To check for the presence of this sign, the nurse would do which of the following?
- Ask the client to extend their arms
- Check for the presence of Homan’s sign
- Instruct the client to lean forward
- Measure the client’s abdominal girth
Rationalization
When caring for a client with ascites the nurse should understand that the portal vein:
- Brings blood away from the liver
- Enters the superior vena cava from the cranium
- Brings venous blood from the intestinal wall to the liver
- Is located superficially on the anteromedial surface of the thigh
Rationalization
The nurse administers Neomycin to a client with hepatic encephalopathy, understanding its therapeutic effect is achieved by:
- Killing bacteria
- Preventing ammonia formation
- Improving asterixis
- None of the above
Rationalization
A nurse provides dietary instructions to a client with a diagnosis of cholecystitis. Which of the following food items identified by the client indicates an understanding of foods to avoid?
- Fresh fruit
- Fresh vegetables
- Poultry without skin
- Brown gravy
Rationalization
An ambulatory care nurse is preparing a client scheduled for a liver biopsy., The nurse reviews the client’s record and expects to note which of the following laboratory results documented in the client’s chart in preparation for this procedure?
- Prothrombin time
- White blood cell count
- Blood urea nitrogen
- Uric acid level
Rationalization
The patient has been treated for a peptic ulcer. He enters the hospital reporting that he has vomited a very large amount of blood. The nurse should expect which sign to be present?
- Decreased blood pressure
- Decreased pulse
- Decreased respirations
- Increased urinary output
Rationalization
When caring for a patient after open cholecystectomy, the nurse should be aware of the major complication of procedure which is:
- Hemorrhage
- Atelectasis
- Wound dehiscence
- Infection
Rationalization
The nurse is assessing a male client after 24 hours following a cholecystectomy. The nurse noted that the T-tube has drained 500 mL of green-brown drainage since the surgery. Which nursing intervention is appropriate?
- Clamp the T-tube
- Irrigate the T-tube
- Notify the physician
- Document the findings
Rationalization
During abdominal examination, the nurse notices bluish discoloration of the periumbilical area. This indicates pancreatic bleeding and is referred to as:
- Grey-Turner’s sign
- Cullen’s sign
- Battle’s sign
- Kernig’s sign
Rationalization
An ineffective nursing measure to prevent the progress of hepatic coma is:
- Giving diuretics
- Making certain that a low-protein diet is served
- Assessing if there is adequate renal perfusion
- Assessing for a patent airway and oxygenation
Rationalization
Which of the following instructions is appropriate for a nurse to give to a patient who has gastroesophageal reflux disease (GERD)?
- Take prescribed antacids before eating
- Place blocks under the legs of the head of the bed
- Eat a high-fat, low-protein diet
- Lie down for one hour after eating
Rationalization
The nurse attempts to prevent the occurrence of reflux and heartburn.
- Antacids are given after meals, usually 30 to 60 minutes post cebum in order to give time for gastric secretions to be released before administering the antacid to neutralize them.
- The use of a reverse Trendelenburg position uses gravity to reduce the occurrence of reflux.
- A high-fat diet will enhance gastric acid production.
- Lying down after eating will allow gastric contents to flow upwards, worsening heartburn.
A nurse would assess a patient who has undergone a total gastrectomy for early symptoms of dumping syndrome, which include which of the following?
- Diaphoresis and lightheadedness
- Facial flushing and paresthesia
- Disorientation and vomiting
- Diarrhea and abdominal distention
Rationalization
1
A total gastrectomy will predispose the patient to dumping syndrome, wherein gastric contents rapidly empty into the intestine. The presence of glucose in the gastric contents draw water into the intestines to produce diarrhea. However, option 4 contains abdominal distention, which is not included. The water drawn into the intestines reduces total blood volume, which results in diaphoresis and lightheadedness.
Which of the following statements, if made by a patient who has diverticulitis, would indicate to a nurse that the patient is following the diet plan correctly?
- I eat meat five times a week
- I do not eat fried foods
- I drink decaffeinated coffee
- I eat green salad every day
Rationalization
4
Diverticulosis is a condition characterized by the formation of diverticula in the colon, small outpouching of the colon. This is normally asymptomatic, but can result in diverticulitis once the pouches become inflamed.
Option 4 tackles the risk factor of constipation implicated in the development of diverticula.
A nurse should expect a Sengstaken-Blakemore tube to be ordered for a patient who has bleeding esophageal varices in order to:
- Cause vasoconstriction of the splenic artery
- Ensure airway potency
- Provide for enteral nutrition
- Apply direct pressure to the area
Rationalization
4
A Sengstaken-Blakemore tube is a triple-lumen tube that is inserted into the esophagus to compress the blood vessels to prevent bleeding.
Which of the following factors, if noted in a patient’s history, would indicate a predisposition for developing cholecystitis?
- Obesity
- Hypertension
- Depression
- Childlessness
Rationalization
1
Cholecystitis is an inflammation of the gallbladder. Its main risk factors are the presence of gallstones (cholelithiasis). For cholelithiasis, the four main risk factors (4 Fs) include being female, fat, forty and above, and/or fertile.
A client with cirrhosis may have alterations in which of the following laboratory values?
- Carbon dioxide level
- ALT
- pH
- Erythropoietin
Rationalization
- CO2 is implicated in lung problems.
- ALT is a liver enzyme, which becomes elevated in liver injury.
- pH can be affected by many systems, mainly the lungs and kidneys.
- Erythropoietin is produced by the kidneys.
A client with acute pancreatitis asks the nurse, “When will I be able to eat again?” The most appropriate response by the nurse is
- “If you do not have the infection in the pancreas anymore.”
- “When the doctors order for it.”
- “When your blood test for enzymes improves.”
- “Maybe after a week.”
Rationalization
3
Acute pancreatitis is diagnosed by increasing pancreatic enzyme levels. This includes lipases (more destructive) and amylase. Conversely, the reduction of these enzymes indicate the resolution of disease and signal tolerance for the original diet (Option 3)
The nurse would expect which of these assessment findings in a client with duodenal ulcers?
- Epigastric pain occurring at night
- Distended abdomen
- Epigastric pain relieved by vomiting
- Positive fluid wave
Rationalization
- Epigastric pain at night is found in duodenal ulcers as gastric emptying continues at night, and irritates the duodenum. Eating at night when pain occurs closes the pylorus, which relieves pain.
- A distended abdomen is a complication, but is not expected.
- Epigastric pain relieved by vomiting is seen in gastric ulcers.
- A positive fluid wave is seen in ascites.
The client has had a total gastrectomy. The nurse should teach the client about the necessary long-term treatment for which of these conditions?
- Vitamin K deficiency
- Vitamin A deficiency
- Vitamin B12 deficiency
- Vitamin C deficiency
Rationalization
3
The removal of the entire stomach, especially its lower end, removes the parietal cells that produce intrinsic factor, a vital substance in the absorption of Vitamin B12. This results in Vit. B12 deficiency that can cause pernicious anemia.
In caring for a client with hiatal hernia, which of the following should be included in a teaching plan regarding the causes?
- Avoid heavy lifting
- Dietary plan based on soft foods
- Prevalence in young adults
- Prevalence in fair-skinned individuals
Rationalization
1
Hiatal herniation occurs due to increased intraabdominal pressure, which pushes the stomach upwards, causing gastroesophageal reflux and pain. Heavy lifting requires bracing the core of the body, increasing intraabdominal pressure.
The most fatal complication of choledocholithiasis is ascending cholangitis which may complicate to develop what type of shock?
- Hypovolemic Shock
- Septic Shock
- Anaphylactic Shock
- Neurogenic Shock
Rationalization
2
Choledocholithiasis is stone formation in the common bile duct. This can result in obstruction, and bile is unable to exit, and produces jaundice and pain in the right upper quadrant of the abdomen. After obstruction, the common bile duct can become traversable by bacteria in the small intestine, which is what “ascending cholangitis” refers to. This infection incites a fever, completing Charcot’s Triad of Ascending Cholangitis: jaundice, RUQ pain, and fever.
All in all, this puts the patient at risk for septic shock once the patient displays Charcot’s triad, hypotension, and confusion. All together, this is known as Reynold’s Pentad.
A client with liver cirrhosis has severe ascites and is experiencing difficulty of breathing. Which of the following is the priority nursing intervention?
- Prepare for paracentesis
- Administer diuretics as ordered
- Place the client in a reverse Trendelenburg position
- All of the above
Rationalization
3
Difficulty of breathing in a patient is caused by pressure on the diaphragm from the collection of fluid in the peritoneum. The priority action to take is to utilize a reverse Trendelenburg position to localize the fluid to the bottom of the peritoneum.
After pyloroplasty, which of the following interventions prevent rapid gastric emptying?
- Simple sugar in the diet
- Low protein intake
- Liquid must be taken in between meals
- All of the above
Rationalization
3
A pyloroplasty repairs the pylorus by widening the pyloric sphincter. This puts the client at risk for dumping syndrome, which is promoted by simple sugars or carbohydrates in general (eliminate Option 1). Fluids also promote gastric emptying, which contribute to the pathophysiology of dumping syndrome.
In patients with dumping syndrome, the following diet is followed:
- Low carbohydrates; restrict simple sugars
- High protein, which aids in preventing fluid shifting (prevent diarrhea)
- Moderate fat content to promote slow gastric emptying
A client with possible appendicitis is being assessed. Which of the following is not contraindicated in this client?
- Cleansing enema
- Digital rectal examination
- Warm compress
- None of the above
Rationalization
2
A digital rectal exam does not reach deep enough to affect the appendix, and is therefore not contraindicated. Any enema will put the patient with appendicitis at risk for rupture. Warm compresses, which promote vasodilation and therefore increases swelling, also increases the risk for rupture. Additionally, laxatives also promote rupturing.
The “I” in “IBS” refers to which word?
- Irritable
- Inflammatory
- Infectious
- Incredible
Rationalization
- IBS stands for Irritable Bowel Syndrome.
A clinic nurse is providing health teaching for a patient with newly diagnosed gastroesophageal reflux disease (GERD). Which of the following is an inappropriate teaching to provide to the patient?
- Change dietary patterns to small frequent feedings with a bedtime snack
- Avoid wearing tight clothing
- Use magnesium carbonate (Gaviscon) to neutralize acidity
- Avoid bending, stopping, or slumping postures
Rationalization
1
While small frequent feedings is correct, a bedtime snack is not suggested as this stimulates digestive processes at bedtime, which predisposes the patient lying down to experience heartburn.
Postoperatively, the patient develops dumping syndrome. Which of the following statements, if made by the patient, should indicate the need for further dietary teaching?
- “I should eat bread with each meal.”
- “I should eat smaller meals more frequently.”
- “I should lie down after eating.”
- “I should avoid drinking fluids with my meals.”
Rationalization
1
Dumping syndrome is enhanced by carbohydrates as these stimulate rapid gastric emptying. Therefore, option 1 is incorrect. The patient should eat smaller meals, lie down after eating (to reduce the effect of gravity on gastric emptying), and avoid fluids with meals.
A client with peptic ulcer in the duodenum would probably describe the associated pain as:
- An ache radiating to their left side
- An intermittent colicky flank pain
- A gnawing sensation relieved by food
- A generalized abdominal pain intensified by moving
Rationalization
3
The pain produced by a duodenal ulcer is epigastric in location; not radiating, flank, or generalized. Additionally, eating food closes the pylorus, which relieves irritation of the duodenum.
A nurse is providing instructions to a client about measures to minimize the risk of dumping syndrome. The nurse tells the client to do which of the following?
- Increase fluid intake, particularly at mealtime
- Maintain a high-carbohydrate diet
- Maintain a low-Fowler’s position while eating
- Ambulate for at least 30 minutes after each meal
Rationalization
3
Options 1, 2 and 4 all enhance gastric emptying. A low-Fowler’s position reduces the effects of gravity on gastric emptying, reducing the severity of dumping syndrome.
A client being treated for esophageal varices has a Sengstaken-Blakemore tube inserted to control the bleeding. The most important assessment is for the nurse to:
- Check that a hemostat is at the bedside
- Monitor IV fluids for the shift
- Regularly assess respiratory status
- Check that the balloon is deflated on a regular basis
Rationalization
3
The nurse prioritizes the airway (refer to the ABCs of Life), especially in the context of a Sengstaken-Blakemore tube as the esophagus runs parallel posterior to the trachea.