Mainly based on Sir V’s lectures on high-risk pregnancies and disorders of pregnancy. A high-risk pregnancy is one in which the mother or fetus has a significantly increased harm, damage, injury, or disability, and loss of life or death. It often requires specialized care from specially trained healthcare providers in specialized facilities.
Related Notes
Bleeding Disorders of Pregnancy
Bleeding at any time of pregnancy is a major sign of danger except for SHOW, which is a sign of true labor and is the only time bleeding is expected. Possible causes of bleeding are categorized according to its trimester:
| Trimester | Causes of Bleeding |
|---|---|
| First | Abortion, Ectopic Pregnancy |
| Second | Abortion (up to 20 weeks), Incompetent Cervix, Hydatidiform Mole |
| Third | Abruptio Placenta, Placenta Previa |
Abortion
An abortion is the termination of a pregnancy before the age of viability, currently at 20 weeks of gestation. Abortions are generally divided between those that are induced, and those that are spontaneous. Two types of induced abortions are the following:
- Therapeutic Abortion: AKA Legal Abortion, to save the life of the mother. This may be used in cases such as ectopic pregnancies, and gravido cardia.
- Non-Therapeutic Abortion: AKA Criminal Abortion, to get rid of unwanted pregnancies. These are commonly performed through “Hilot”, midwives, doctors, then nurses. While the others perform that abortive procedure, nurses often suggest an abortive drug. Cytotec is a commonly used abortifacient. It is an antiulcer drug taken orally or used as a vaginal suppository.
- When used as a vaginal suppository, cytotec changes the pH balance of the vagina, leading to ascending infection, resulting in chorioamnionitis. The amniotic fluid becomes infected, which the fetus also contracts. The uterus contracts, separating the placenta from the body to prevent infection, resulting in abortion.
- When used orally (overdose amount), it induces uterine contractions. If underdosed, it may fail to abort the fetus but still result in congenital defects. This commonly results in anencephaly.
Spontaneous Abortions
A spontaneous abortion occurs without medical or mechanical intervention. An abortion may present with signs of vaginal bleeding or spotting, uterine/abdominal cramps, passage of tissues or products of conception, and signs related to blood loss/shock (pallor, tachycardia, tachypnea, cool clammy skin, restlessness, oliguria, air hunger, and hypotension). There are six types:
flowchart TB
1(Threatened Abortion)-->2
2(Imminent Abortion)-->3
2-->4
3(Incomplete Abortion)-->6
3-->4
4(Complete Abortion)
5(Missed Abortion)-->6
6(Septic Abortion)
- Threatened Abortion: the only form of abortion where the pregnancy may still be saved. The only presenting signs in a threatened abortion are contractions or abdominal cramping and spotting.
- Imminent Abortion: progression of threatened abortion to an unrecoverable state. This will result in a complete or incomplete abortion.
- Complete Abortion: complete expulsion of all the products of conception. The abortion is done, and further care is focused on postpartum care.
- Incomplete Abortion: a remnant of the products of conception is left in the uterus. This may progress to sepsis.
- Missed Abortion: intrauterine fetal demise (IUFD); the fetus may remain in the uterus for 4 to 6 weeks without leading into complications (sepsis). The mother often reports that there have been no fetal movements, prompting the nurse to auscultate and find no fetal heart tone. The best diagnostic examination is an ultrasound.
- Septic Abortion: may result from incomplete or missed abortions. Discharge is foul and brown in color.
(According to Sir V.)
| Spontaneous Abortions | Bleeding/ Contractions | Cervical Dilatation | B.O.W. | Tissues Passed | Fever |
|---|---|---|---|---|---|
| Threatened | Mild | Closed | (+) | None | No |
| Inevitable | Moderate – Strong | Open, especially inevitable if >3 cm | (–) | None | No |
| Complete | Mild – None | Close or partially open if recent | (–) | Complete placenta with fetus | No |
| Incomplete | Moderate – Strong | Open | (–) | Placenta/ Fragments | No |
| Missed | None | Closed before infection | (+) before infection | None | No |
| Septic | Moderate – Strong | Open | (–) | Either; foul discharge | Yes |
| Spontaneous Abortions | Management | Medication |
|---|---|---|
| Threatened | - No Internal Examinations for any type of bleeding, as this causes further irritation and bleeding. - Sex is disallowed. - External fetal monitoring is done. - Complete bed rest. - Watchful waiting; save pads for monitoring discharge. | - Tocolytic - Sedatives, especially for an emotionally distressed patient. |
| Inevitable | Admission/Hospitalization | |
| Complete | Pericare, etc. | Oxytocic Analgesics Antibiotics |
| Incomplete | Dilatation and Curettage | Oxytocic Analgesics Antibiotics |
| Missed | Delivery of abortus Dilatation and Curettage | Oxytocic Analgesics Antibiotics |
| Septic | Dilatation and Curettage | Oxytocic Analgesics Antibiotics Antipyretics Antiinflammatories |
| Habitual |
(According to Dr. RPS)
| Spontaneous Abortions | Bleeding | Abdominal Cramps | Cervical Dilatation | Tissue Passage | Fever |
|---|---|---|---|---|---|
| Threatened | Slight | May or may not be present | None | None | No |
| Inevitable | Moderate | Moderate | Open | None | No |
| Complete | Small to negative | Moderate | Close or partially open | Complete placenta with fetus | No |
| Incomplete | Severe (bleeds the most) | Severe | Open with tissue in cervix | Fetal or incomplete placental tissue | No |
| Missed | None to severe incoagulopathy | None; No FHT with UTZ | None | None | No |
| Septic | Mild to severe | Severe | Close or open with or without tissue | Possible; foul discharge | Yes |
Habitual Abortion
Three or more consecutive abortions can be considered habitual or recurrent. This is most commonly caused by an incompetent cervix, and occurs as any of the types of spontaneous abortions mentioned above. This is often detected in the threatened phase, and cervical closure (cerclage, cervical stitching) is done. If the cause of habitual abortion is not due to an incompetent cervix, determination of the etiology and treatment of the underlying cause is done.
Additional nursing care/management from Dr. RPS for Threatened and Inevitable Abortions
| Type | Nursing Care/Management |
|---|---|
| Threatened Abortion | - Advise complete bedrest for 24 to 48 hours. - Teach to save all blood clots passed and perineal pads used. - Advise prompt reporting to the hospital if bleeding persists or increases. - Prevention of abortion: avoid coitus or orgasm, especially around the normal time of menstrual period. |
| Inevitable Abortion | - Save or monitor clots, pads, or tissues for a correct diagnosis. - Monitor VS, blood loss, I&O, changes in status, and signs of infection, and refer any deviation. - Institute measures to treat shock as necessary: replace blood, plasma, and fluids as ordered. - Prepare for surgery. - Provide psychological support: non-judgmental attitude, encourage verbalization, reduce anxiety, and allow the patient to cry. - Prevent isoimmunization: administer RhoGAM as ordered if: the mother is Rh negative; the abortus is Rh positive, and Coombs test result is negative. |
Incompetent Cervix
A condition characterized by a mechanical defect in the cervix causing cervical effacement, dilation, and expulsion of the products of conception in the mid-trimester of pregnancy. Pregnant women are at risk for an incompetent cervix if they (a) have a congenital defect of the cervix (short cervix), (b) trauma to the cervix as in forceful dilatation, curettage, and difficult delivery, and (c) cervical lacerations procedures (conization, cauterization).
This appears as:
- Painless contractions resulting in the delivery of a dead or non-viable fetus
- History of abortions (habitual abortion)
- Finding of a relaxed cervical os on pelvic examination
Treatment and Nursing Management
Cervical cerclage during the 14th and 16th week of gestation or prior to the next surgery. A suture or ribbon is placed beneath the cervical mucosa to close the cervix during pregnancy to help prevent pregnancy loss or premature birth. This may be done via:
- Shirodkar-Barter Cerclage: a permanent suturing of the cervix, with future pregnancies delivered via cesarean section.
- McDonald Cerclage: a temporary purse-string suturing of the cervix removed at term in preparation for a vaginal delivery.
Ectopic Pregnancy
An ectopic pregnancy is a condition where pregnancy develops outside of the uterine cavity: extrauterine pregnancy in which the blastocyst implants anywhere other than the endometrial lining of the uterine cavity. Nearly 95% of ectopic pregnancies implant in the fallopian tube most commonly as a mechanism of abnormal fallopian tube anatomy that alters normal embryo transport.
The two leading predisposing factors for an ectopic pregnancy is PID and IUD use. PID can affect the cervix, ovaries, and fallopian tubes. The IUD commonly only affects the fallopian tubes (e.g. salphingitis).
- Scar formation post-infection/inflammation results in obstruction of embryo transport. Stuck at the ampulla or other parts of the fallopian tube, it may become an extrauterine pregnancy.
- IUDs, most commonly the Copper-T variant, attracts sperm until they die. If displaced, sperm may enter the fallopian tube, but the formed zygote will not be able to exit. This results in an interstitial ectopic pregnancy
There are four main types of ectopic pregnancies based on the location of extrauterine implantation:
- Tubal Ectopic Pregnancy: the most common form. The fallopian tubes rupture by 10 to 12 weeks because of their thinness. There are further classifications of tubal implantation based on the segment of the fallopian tube:
- Ampullary Implantation: the most common, but is comparatively safer as only the fallopian tube is damaged in case of rupture and in treatment.
- Interstitial Implantation: the more dangerous form, as the interstitial segment is the narrowest portion and is directly connected to the uterus, crossing the perimetrium, myometrium, and the endometrium. The uterus is also partially damaged.
- Ovarian Ectopic Pregnancy
- Abdominal Ectopic Pregnancy: the most dangerous form of ectopic pregnancy because of the involvement of abdominal organs. Implantation occurring on organs may damage the organ.
- Cervical Ectopic Pregnancy: a rare variant, and is the safest. Management is through administration of methotrexate. A D&C is not viable as the cervix is friable— easily bleeds.
Signs of Rupture
- Kehr’s Sign is the earliest sign of rupture, a sudden sharp stabbing pain from the low abdomen radiating to the shoulder or neck.
- Cullen’s Sign is the following sign of rupture, a bluish discoloration of the periumbilical area indicating pooling of blood.
- Shock is a late sign, appearing from the loss of circulating blood volume. Signs include cool clammy skin, tachycardia, tachypnea, hypovolemia, hypotension, and hypothermia.
Diagnosis of Ectopic Pregnancies
Diagnosis starts with clinical signs. Ectopic pregnancy is considered in any reproductive-aged woman with pain, uterine bleeding, and/or anemia.
- Ultrasonography is the study of choice for ectopic pregnancy. The initial ultrasound for a pregnant woman confirms the pregnancy, locates the pregnancy, and locates the placenta.
Management
In an unruptured ectopic pregnancy and in cervical implantations, methotrexate may be used to induce the separation of the abortus. Otherwise, resection/removal of the abortus and its affected site is done, e.g., a salpingectomy, oophorectomy, etc.
Complications of an Ectopic Pregnancy
- Hemorrhage
- Infection
- Rh Sensitization: RhoGAM prevents isoimmunization and is given to an Rh-negative mother with an Rh-positive ectopic pregnancy with a negative Coombs test.
Hydatidiform Mole
AKA Gestational Trophoblastic Disease (GTD). An H-mole is a benign neoplasm of the chorion. The chorion fails to develop into a full-term placenta and instead degenerates into fluid-filled vesicles. Its actual cause is unknown, but risk factors include:
- Faulty fertilization, one of each sex cells are required e.g. two sperms fertilize one egg
- Low socio-economic standing
- Protein deficiency: the building blocks of tissues; poor protein content results in the death of the blastocele, which, if not removed, will multiply and create fluid filled vesicles rapidly.
- The vesicles rupture from the 16th to 20th week of pregnancy. The resulting discharge is foul and brown.
Classical Signs
- Bigger-than-date uterus due to rapid proliferation of blastocele
- HCG is abnormally high: 1,000,000 to 2,000,000 IU/L/24 hours. Its normal value is 50,000 to 400,000 IU/L/24 hours.
- Absence of fetal signs: outline (via ultrasound), heart rate, movement
- Passage of vesicles: confirmatory for H. mole
Management
If no spontaneous evacuation occurs, the best option for management is a D&C done with a curette then ovum forceps followed by suction curettage via large-bore catheter with low-force suctioning. A hysterectomy may also be done if no future pregnancies are desired, or if hCG remains elevated.
- Afterwards, hCG titer is done to see if remnants were left. If remnants are present, hCG remains high.
- Pregnancy should be avoided for at least one year to prevent another H. Mole pregnancy, as this may also result in choriocarcinoma (also treated with methotrexate).
Prognosis, Complications
80% of patients experience remission after D&C of the H-mole. However, the chorion may become cancerous; a choriocarcinoma. This is the most dreaded complication. Other complications includes:
- Hemorrhage: most serious during the early treatment phase
- Uterine perforation
- Infection
Placenta Previa
The premature separation of an abnormally low implanted placenta. This is the most common cause of bleeding in the third trimester, occurring in 1:150 to 1:200 pregnancies. Risk factors for placenta previa include:
- Multiparity (high partiy): the single most important factor
- Upper uterine segment dysfunction: decreased vascularity, scarring, tumors
- Advanced maternal age: >35 years
- Multiple pregnancy
The patient will exhibit the following signs and symptoms:
- Painless vaginal bleeding of bright red, fresh blood in the third trimester (7th month). This may be slight or profuse coming after an activity, coitus, or internal examination.
- Soft, flaccid uterus with intermittent hardening if in labor.
- Intermittent pain if placenta previa occurs secondary to uterine contractions in labor.
The determination of placenta previa is imaging through ultrasonography, giving a 95% accurate result and detects the site of the placenta done early in the pregnancy.
Vaginal Delivery with a Previa
When the placental tip measures between 1 and 12 cm from the internal cervical os, up to 90% of these patients will deliver successfully via the vaginal route. As long as the inferior margin of the placenta is at least 2 cm from the internal os, there is no significant increased risk of bleeding during labor.
Abruptio Placenta
An abruptio placenta is a complication of late pregnancy or labor characterized by premature partial or complete separation of a normally implanted placenta; also termed as accidental hemorrhage and ablatio placenta. This is the second leading cause of bleeding in the third trimester; occurring in 1:300 pregnancies second only to placenta previa. Risk factors for abruptio placenta include:
- Maternal hypertension; PIH (#1), renal disease
- Sudden uterine decompression such as in polyhydramnios and multiple gestation.
- Advanced age
- Multiparity
- Short umbilical cord: double cord-coil
- Trauma (#2); fibrin defects
- Inappropriate use of oxytocin
- Infection
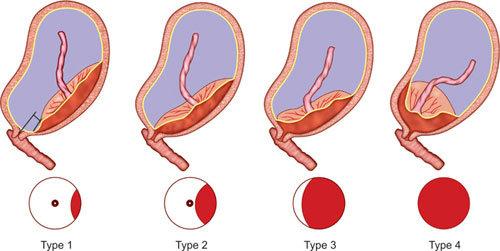
| Types | Description |
|---|---|
| Type I | Classic concealed, covert, central type. The placenta separates at the center (schultz), causing blood to accumulate behind the placenta, hiding the presence of bleeding. External bleeding does not appear to match the severity of shock. |
| Type II | Marginal, overt, external bleeding type. The placenta separates at the margins (duncan), allowing old blood (dark red, brown) to spill out. In this type, external bleeding matches the severity of shock. |
| Type III | Mixed. Some part of the blood remains concealed, while some are expelled. |
Assessment Findings and Diagnosis
- Painful vaginal bleeding in the third trimester.
- Rigid, board-like, and painful abdomen.
- Enlarged uterus from concealed bleeding; signs of shock that may be disproportional to external bleeding.
- Tetanic contractions if in labor— alternating contraction and relaxation does not occur.
Diagnosis is based on clinical signs and symptoms and an ultrasound to image retroplacental bleeding.
| Areas of Major Differences | Placenta Previa | Abruptio Placenta |
|---|---|---|
| Placental Location | Lower uterus | Upper uterus |
| Bleeding | Painless, vaginal, fresh, bright red | Painful, often concealed, dark, old blood if external |
| Abdomen | Soft/flaccid; during labor with intermittent hardening and softening corresponding with uterine contractions. | Hard, board-like; during labor, No characteristic intermittent hardening and softening of the abdomen. |
| Major Complications | Hemorrhage Prematurity Obstruction of the birth canal | Hemorrhage Couvelaire Uterus Disseminated Intravascular Coagulation (DIC) |
| PIH as a risk factor | PIH is not a risk factor | PIH is a major risk factor |
Clotting studies reveal the presence of DIC and clotting defects. The thromboplastin from the retroplacental clot enters maternal circulation and consumes maternal free fibrinogen, resulting in DIC and hypofibrinogemia.
Management for both Placenta Previa and Abruptio Placenta
- No Internal Examination; external fetal monitoring
- Watchful Waiting
- Cesarean Section. AP may result in fetal distress faster than PP.
- Coomb’s Testing
Rh Incompatibility
An Rh incompatibility can be a cause of hemolysis (and pathologic neonatal jaundice). This is common in cases where the mother is Rh negative, while the fetus or the husband is Rh positive. In a standard pregnancy, the fetal blood is separated from the mother’s blood by the placental barrier. The fetal blood occupies the placenta and the fetal body. The exchange of required substances between the mother and fetus occurs through means of diffusion and osmosis, transferring oxygen, carbon dioxide, antibodies, proteins, viruses, etc.
In case, during delivery, a first occurrence of Rh-negative maternal blood and Rh-positive fetal blood mix such as in a Schultz-mechanism placental abruption, the mother’s immune system detects the Rh-positive blood and produces antibodies to destroy the foreign Rh-positive fetal blood. The newborn, if delivered, is not in danger of hemolysis by the antibodies. However, in a second pregnancy, this would introduce problems as the mother’s antibodies enter the fetal Rh-positive blood, causing hemolysis.
Coombs Test
A test to determine if the mother produced any antibodies against Rh-positive blood. A positive Coombs result indicates agglutination and therefore the presence of antibodies. If it is negative, no antibodies were produced.
- Direct Coombs Testing: fetal blood is used as a sample.
- Indirect Coombs Testing: maternal blood is used as a sample. This is more common because maternal blood is easier to obtain.
If the Coombs test is negative and the mother has a possibility of another Rh-positive fetus, RhoGAM is given to prevent the formation of antibodies, given within 72 hours of delivery.
However, if the Coombs test is positive, a blood transfusion may be used to save the pregnancy with an intrauterine external blood transfusion (IUEBT). The blood type used may be O-, heparinized due to the delicacy of the procedure. Despite this, some mild hemolytic reactions may still occur, resulting in pathologic jaundice at birth.
Cardiac Disease in Pregnancy
Also known as gravidocardiac patients, these are pregnant women who experience heart disease during pregnancy. The most common predisposing factor is rheumatic heart disease caused by rheumatic fever secondary to respiratory infection by Group A Beta-Hemolytic Streptococcus.
- The affected side of the heart is the left side, as oxygenated blood from pulmonary circulation returns to the left atrium, resulting in carditis. Adherence of some microorganisms to the mitral valve results in inflammation of the mitral valve, swelling occurs, resulting in mitral valve prolapse.
- The antibiotic drug of choice for GABHS is Penicillin. Late administration still cures the infection, but scarring may occur on the mitral valve. Hardening of the mitral valve leads to inability to close, resulting in continuous blood flow. This permanent damage, mitral valve stenosis, leads to gravid cardiac patients.
- GABHS may also result from dental caries, which contain Staphylococcus aureus and Streptococcus. It may be transferred from men to women through oral contact as well. Oral care should be marked as important.
Blood volume increases by 30 to 50% in pregnancy. Due to the damage to the mitral valve, hypertrophy of the heart occurs, leading to weakening of the left ventricle (decreased pumping ability), resulting in left-sided congestive heart failure with pulmonary congestion (edema). Cardiac arrest may occur, resulting in death.
| Type | S/S | Damage | Activity Level | Activity Limitation | Delivery |
|---|---|---|---|---|---|
| I | (–) | Very minimal | None | None | NSD |
| II | (+) | Minimal | Heavy | Slight Limitation | NSD/Forcep |
| III | (+) | Moderate | Light | Marked Limitation | Forcep/Abortion |
| IV | (+) | Severe | At rest | Complete Bed Rest | Forcep/Abortion |
Signs and symptoms include difficulty of breathing, palpitations, easy fatiguability, chest pain, etc.
- “Activity Level” denotes the level of activity required to produce the signs and symptoms.
- S/S refers to the presence of symptoms, i.e., only Type I gravidocardiac patients are asymptomatic.
Forcep Delivery
Forcep deliveries are guided deliveries that are done with epidural anesthesia, with a ruptured bag of water, fully dilated cervix, and a fully effaced cervix, as the baby descends with positive station. There are two types:
- Mid Forcep Delivery: +1 - +2
- Low Forcep Delivery: +3 - +4
Rheumatic Fever
An infection involving the heart, CNS, joints, subcutaneous tissue, and the skin caused by Group A Beta-hemolytic Streptococcus.
Jones Criteria
A diagnosis of rheumatic fever presents with two major manifestations or one major with two minor manifestations.
- Major: heart carditis, CNS chorea, joint polyarthritis, subcutaneous nodules, skin erythema marginatum.
- Minor: fever, history of strep. infection (ask for sore throat), elevated laboratory findings (anti-streptolysin O titer [ASOT]), arthralgia
- ASOT Lab Findings:
- 150 to 250 Todds unit: normal
- >250 to <500 Todds unit: Dormant RF
- >500 to <5000 Todds unit: Active RF
- >5000 Todds unit: Rheumatic Heart Disease
- ESR, increased during hyperemia then decreased later in congestive heart failure.
- CRP, produced by the liver in response to inflammation and tissue damage and is therefore increased. This is used to determine both the presence of inflammation and response to treatment.
- ASOT Lab Findings:
Pathophysiology
- Spread of GABHS to the pulmonary system, through pulmonary circulation, to the mitral valve (proliferation) of the heart results in the major manifestations to the heart, brain, joints, subcutaneous tissue, and skin:
- Carditis
- Chorea
- Polyarthritis
- Subcutaneous Nodules
- Erythematous Marginatum
- Mitral Valve Stenosis: damage to the mitral valve from GAHBS. Left ventricular hypertrophy occurs for compensation. This backs up to the left atrium and pulmonary circulation, resulting in LSCHF. Crackles and moist coughing occurs from pulmonary edema.
- Lanoxin (Digitalis) increases heart contraction, while decreasing heart rate. This results in bradycardia. Do not administer Lanoxin if heart rate is bradycardic. Decreased cerebral perfusion alters LOC.
Nursing Management
- Fever, Pain (polyarthritis), Inflammation, Thrombotic Formation
- Aspirin fulfills all of these problems within a child (antipyretic, analgesic, antiinflammatory effect, thrombolytic effect). The main purpose is for its antiinflammatory effect on polyarthritis.
- Diet: high calorie, high fiber, low sodium, and soft diet. If polyarthritis affects the temporomandibular joint, NGT/OF may be required.
- Polyarthritis: pain may be produced even by thin linens. A bed cradle is created and formed as a tent, to maintain thermoregulation without placing weight on the patient directly.
- Fractured TSB may be required to reduce discomfort. Avoid the joints, and only pat the patient. Place a moist towel on the forehead, torso, and axillary areas.
Treatment
Penicillin is the drug of choice, combined with erythromycin (oral) and benzathine penicillin (IM). 2. Oral: Erythromycin with Penicillin 3. Monthly injection of 1 gram benzathine penicillin (twice a month, 500 mg per dose).
Pregnancy-Induced Hypertension
A disorder characterized by proteinuria, edema, and hypertension appearing after the 20th to 24th week of pregnancy and disappearing 6 weeks after delivery. This occurs in 7% to 10% of all pregnancies and is one of the major causes of maternal and neonatal mortality. Its actual cause is unknown, but often involves arterial vasospasms in response to maternal hormones.
- Etiologic Factors:
- Nulliparity, with extremes of age (<18, >35)
- High Parity
- Severe nutritional deficiency: low protein and low calorie diet
- Coexisting conditions: diabetes mellitus, multiple pregnancies, polyhydramnios, chronic hypertension, renal disease, atherosclerosis/arteriosclerosis in older patients.
| Type | B.P. | Onset | Proteinuria | Edema | Seizures |
|---|---|---|---|---|---|
| Gestational Hypertension | >140/90 | >20 weeks | (–) | (–) | (–) |
| Mild Preeclampsia | >140/90 | >20 weeks | +1 - +2 (>300 mg/d) | Mild – Mod | (–) |
| Severe Preeclampsia | >160/110 | >20 weeks | +3 - +4 (>500 mg/d) | Generalized | (–) |
| Eclampsia | >160/110 | >20 weeks | +3 - +4 (>500 mg/d) | Generalized | (+) |
| Chronic Hypertension | >140/90 | <20 weeks | (–) | (–) | (–) |
Management
- Promote safety
- Maternal Well Being: monitor BP and Weight Gain daily.
- Monitor for Edema: check the ankles for pitting; edema grading (+, ++, +++, ++++) → +2 mm for each (+)
- Monitor SGPT, SGOT for hepatic involvement
- Monitor BUN and Creatinine to monitor kidney function
- Fetal Well Being:
- Monitor FHR: 120 - 160 BPM; tachycardia is an early sign of fetal distress.
- Monitor Kick Counts: 5 to 15, normal is 10; hyperactivity is an early sign of fetal distress, followed by hypoactivity.
- Perform an UTZ to check for IUGR/SGA.
- At the bedside prepare an oxygen tank, suction machine, reflex hammer, and ophthalmoscope for fundoscopic examination.
- Maternal Well Being: monitor BP and Weight Gain daily.
- Pharmacology
- Hydralazine (Apresoline), a vasodilator, is the antihypertensive drug of choice.
- Magnesium Sulfate, an antihypertensive, decreases neuromuscular irritability. It is a CNS depressant.
- Toxicity: hyporeflexia (earliest), bradypnea (<12 RR), oliguria (<30 ml/hr).
- Loading Dose: 6 to 10 grams, usually 6 grams.
- Maintenance Dose: 1 to 2 grams.
- Route: Z-track IM (prevent drug leaking to subcutaneous layer)
- Site: dorsogluteus (upper outer quadrant) injection to accommodate for the large dose.
- Monitor: urine output; urine is the main excretion route of magnesium sulfate metabolites; decreased urine output contributes to hypermagnesemia.
- Antidote: Calcium Gluconate
- Dexamethasone: 6 mg x 4 q 12 hr (bid). Cheaper
- Betamethasone (Celestone): 12 mg x 2 q 24 hr (od). Used for emergency cases due to higher dosage
- Diet Therapy:
- Slightly increased protein (mn. PIH: Protein Is slightly High)
- Decreased fat
- Slightly decreased sodium
Pathophysiology
graph TD
1(Arteriospasm)
2.1(Increased heart workload)
2.2(Increased blood pressure)
3.1(Renal Hypoxia)
3.2(Damaged Glomerular Membrane)
3.3(Increased permeability results in proteinuria)
3.4(Decreased serum colloidal pressure)
3.5(Edema)
1-->2.1
2.1-->2.2
1-->3.1
3.1-->3.2
3.2-->3.3
3.3-->3.4
3.4-->3.5
graph TD
4.1(Hepatic Hypoxia)
4.2(Hepatic Necrosis)
4.3(Hepatic Inflammation)
4.4(Epigastric Pain)
5.1(Cerebral Hypoxia)
5.1.1(Pounding,\nUnrelenting Headaches)
5.1.2(Hyperreflexia)
5.1.3(Visual\nDisturbances)
6(Signs of Impending Seizure)
4.1
4.1-->4.2
4.2-->4.3
4.3-->4.4
5.1-->5.1.1
5.1-->5.1.2
5.1-->5.1.3
4.4--earliest-->6
5.1.1-->6
5.1.2-->6
5.1.3-->6
graph TD
7.1(Uteroplacental Insufficiency)
7.1.1(IUGR)
7.1.2(Fetal Distress)
7.1.3(Abruptio Placenta from placental necrosis)
7.1-->7.1.1
7.1-->7.1.2
7.1-->7.1.3
Gestational Diabetes Mellitus
The most diabetogenic hormone of pregnancy is Human Placental Lactogen (HPL) from the placenta. HPL production in pregnant women start to increase by the sixth month of pregnancy, the best time for screening for GDM.
Diagnosis
- Glucose Challenge Test (GCT) is the screening test, and requires no special preparations. It involves the administration of 50 grams of glucose solution, and one blood extraction an hour after administration.
- Normal result: <145 mg/dL. If this is exceeded, the client must undergo an oral glucose tolerance test.
- Oral Glucose Tolerance Test (OGTT) is the confirmatory test, and requires two days of increased carbohydrate intake followed by NPO post-midnight the day before the exam. Fasting blood sugar is checked and 100 grams of glucose solution is administered, followed by three consecutive blood extractions one hour, two hours, and three hours after the administration.
- Normal FBS: <90 mg/dL
- Normal result 1 hour after administration: <180 mg/dL
- Normal result 2 hours after administration: <155 mg/dL
- Normal result 3 hours after administration: <145 mg/dL
- If two of the four results are abnormal, GDM is diagnosed. If one is abnormal, a repeat test is done. If only one is still abnormal, GDM is negative.
| Parameter | GCT | OGTT |
|---|---|---|
| Purpose | Screening | Confirmatory |
| Preparation | None | Two days of elevated CHO + Fasting post-midnight |
| Administration | 50 g of glucose solution | 100 g of glucose solution |
| Blood Draws | One, 1 hour after | Four |
| Normal Results | <145 mg/dL | - FBS: <90 mg/dL - 1 hour after: <180 mg/dL - 2 hours after: <155 mg/dL - 3 hours after: <145 mg/dL |
| Follow-up | If abnormal, proceed to OGTT | If 2 of 4 are abnormal, confirmation; if only 1 of 4, repeat. |
Assessment Findings
The classical signs of diabetes are present: polyphagia, polydipsia, polyuria. Polyhydramnios may also occur due to the osmotic effect of glucose.
- Insulin function is blocked by HPL. The hyperglycemia results in fluid shifting
- Polyuria results from increased kidney perfusion as a result of fluid shifting.
- Shrinkage of the cells (cellular dehydration) results in polydipsia
- Cellular starvation results in polyphagia, which may result in further hyperglycemia.
- Cellular starvation leads to initiation of gluconeogenesis, which produces ketone bodies (that accumulate in the brain, resulting in decreased level of consciousness, and urine), resulting in diabetic ketoacidosis, then diabetic coma.
- Ketones may also cross the placenta, absorbed by the fetal blood then body and brain (fetal acidosis), causing permanent cognitive impairment.
- Hyperglycemia results in fetal pancreatic hyperinsulinemia and a macrosomic fetus (>4000 grams) that experiences neonatal hypoglycemia (indicated by jitteriness)
- 40 to 60 mg/dL: normal value
- <40 to <35 mg/dL: assess neonatal sucking ability; if absent, prepare IV Glucose Solution, otherwise, provide oral glucose solution (Oresol)
- 35 mg/dL: IV Glucose Solution
Management
- Diet: diabetic exchange diet, balancing meal proportions to manage glucose levels. The patient must consult with a dietitian.
- Exercise: walking is the best exercise. Prior to the exercise, sustaining carbohydrates are required to prevent sudden hypoglycemia.
- Insulin: two types may be added into one insulin syringe (orange hub).
- Self-administration health education:
- Asepsis; what parts of the syringe not to touch, and how to perform handwashing
- Sites of administration: subcutaneous; upper arm, abdomen, thigh, buttocks in 9 or 12 sites two fingerbreadths away from the umbilicus. avoid injection of insulin in the same site due to lipodystrophy.
- Early delivery may be done for diabetic pregnant women with poor glycemic control. As early as 6 weeks (when surfactant production begins), dexamethasone or betamethasone may be given to improve surfactant production for birth.
| Insulin Type | Examples | Onset | Peak | Duration |
|---|---|---|---|---|
| Short-Acting (Regular, Clear) | Humulin R, Novolin R | 30 minutes - 60 minutes | 2 to 4 hours | 6 to 8 hours |
| Intermediate (Cloudy) | NPH | 2 hours | 6 to 8 hours | 12 to 18 hours |
Mixed Insulin Aspiration
The clear (Regular) insulin is aspirated first to prevent contamination of the short-acting insulin with the long-acting insulin. Contamination of regular with intermediate results in changes in duration, while contamination of intermediate of regular results in changes in onset. Changes in duration results in prolonged hypoglycemia, and is a considerable problem. An earlier onset of intermediate insulin is not a cause of concern.
Provide maternal and fetal monitoring:
- Maternal glucose levels
- Maternal blood pressure
- Maternal weight monitoring
- Ultrasound to detect LGA
- Fetal kick count: normally 5 to 15, average 10.
- Chorionic Villi Sampling for detecting chromosomal defects by week 10 to 12.
- Maternal Serum Alpha-Fetoprotein for detecting chromosomal defects and neural tube defects by week 14 to 16.
- Normal findings: 38 to 42 ng/dL. A deficiency may indicate chromosomal defects, while an excess may indicate neural tube defects.
Postpartum Complications
Postpartum Hemorrhage
A postpartum hemorrhage (PPH) is the most common complication after delivery. It is defined as the loss of more than 500 mL of blood after a normal delivery and a loss of more than 1,000 mL of blood after a cesarean section.
Early Postpartum Bleeding
- Atony is the leading cause of postpartum bleeding. It is the inability of the uterus to contract, leading to continued bleeding. It is most commonly caused by an over-distended uterus during pregnancy e.g. from multiple pregnancy, macrosomia, LGA, polyhydramnios, and malpresentation. Other causes include:
- High parity
- Precipitate (<3 hours) or prolonged labor (>24 hours).
- Precipitate labor also results in lacerations. Panting is used rather than pushing.
- Prolonged labor may result in exhaustion.
- Operative Delivery (atony from anesthesia)
- Forceps Delivery
- Management: oxytocin, massage (except if C.S.), early ambulation (not if actively bleeding), bladder emptying, early breastfeeding, and a hysterectomy if necessary.
- Lacerations
- Precipitate Labor
- Powerful Maternal Pushing
- Forceps Delivery (the blade lacerates the perineum)
- LGA
- Breech Presentation
- Management: suturing, antibiotics, analgesics, antiinflammatories, and pericare.
- Retained placental fragments: common in Duncan separation and high-parity women.
- Management: D&C, antibiotics, analgesics, antiinflammatories.
| Condition | Uterus | Blood Color | Origin of Bleeding |
|---|---|---|---|
| Uterine Atony | Relaxed | Dark Red | Uterus |
| Lacerations | Contract | Bright Red | Birth Canal |
| Placental Fragments | Contracted then Relaxes | Dark Red | Uterus |
Late Postpartum Bleeding
Bleeding occuring on the second day postpartum. Subinvolution is a primary cause of late postpartum bleeding, especially due to puerperal sepsis or infection. This is often an ascending infection of the endometrium (endometritis) and is most commonly caused by Staphylococcus aureus, and by Escherichia coli.
- Fever (38°C)
- Lochia is brownish and foul smelling
- Fundus is high (may even be larger due to inflammation)
- Abdominal tenderness
- Management:
- Positioning: Fowler’s to drain infected lochia
- Do not massage the uterus (tenderness)
- Breast feeding and bladder emptying to promote involution
- Antibiotics, analgesia, antiinflammatory, antipyretics
- Perineal care
Diagnostic Examinations
Non-stress and Stress Testing
| Parameter | Non-stress Test | Contraction Stress Test |
|---|---|---|
| Correlation | Fetal Heart Rate to Fetal Activity | Fetal Heart Rate to Uterine Contraction |
| AOG Done | 30th to 32nd week of gestation | 34th to 36th week of gestation |
| Preparation | Breakfast, 30 minutes rest prior to conduction. | 30 minutes rest prior to conduction. Mother is instructed on nipple rolling to stimulate contractions. |
| Findings | Normal findings include a 15 BPM rise in baseline fetal heart rate 10 minutes after fetal activity. Abnormal findings include inadequate or no accelerations after fetal activity. A contraction stress test must be done to investigate further. | Normal findings include no fetal heart rate decelerations— weak contractions should not produce decelerations. Abnormal findings include deceleration even with weak contractions. |
External Fetal Monitor
A deceleration is a distinct decrease below the baseline, with a return to the baseline within 10 minutes. Decelerations are classified by their shape and timing in relation to uterine contractions:
- Early Deceleration (U-shape): decrease, but not below 100 BPM. It occurs early, before acme, and is characterized by a gradual onset at the beginning of a contraction and a slow return to the baseline soon after the contraction ends. This indicates fetal head compression in early contractions and as it enters the birth canal, which stimulates the vagus nerve to decrease FHR. Normally benign; no need for nursing intervention.
- Late Deceleration: usually gradual at onset; the nadir (lowest point) of the deceleration usually occurs after the peak of the contraction; FHR decreases rarely below 100 BPM, but the FHR does not return to baseline by the end of contraction. It is caused by uteroplacental insufficiency, compromising blood flow from the placenta to the fetus; fetal distress. This is an abnormal and ominous sign.
- Variable Deceleration (V-shape or W-shape): occurs at any point. It is believed to be caused mostly by cord compression, featuring abrupt swings in FHT and a rapid return to baseline. It is most frequently observed after rupture of membranes, when there is less amniotic fluid to provide a protective cushion around the cord. While usually not an ominous sign, it requires continuous nursing assessment. The nurse may change maternal positioning to relieve cord compression. If no improvement occurs, administer oxygen, stop oxytocin if infusing, and prepare for an internal examination to identify potential cord prolapse.
| Deceleration | Features | Cause | Action |
|---|---|---|---|
| Early | Before acme; gradual, U-shaped | Fetal Head Compression | Benign; no action required. |
| Variable | Any point; abrupt, V- or W-shaped | Cord Compression | Continuous monitoring; positional adjustment. If improvement is not observed, administer oxygen, stop oxytocin, and prepare for an internal examination for cord prolapse. |
| Late | After acme; gradual | Uteroplacental Insufficiency | Abnormal/Ominous; discontinue oxytocin, position the mother on LLR, give oxygen (8 to 10 L/min), increase hydration, run IV (plain) faster, and prepare for delivery as indicated. |
Ultrasound and Amniocentesis
| Parameter | Ultrasound | Amniocentesis |
|---|---|---|
| Description | Visualization via sound waves. Non-invasive. | Aspiration and analysis of amniotic fluid. Invasive. |
| Preparation | Do not void; if less than five months of gestation, increase oral fluid intake up to 1.5 L of water 90 minutes prior to procedure in order to improve visualization. | Void, as aspiration of at most is done in the lower abdomen, and runs the risk of making contact and injuring the bladder. |
| Purposes | Confirmation of pregnancy, location of implantation and placenta, estimation of amniotic fluid volume, visualization of the fetus, visualization of the calcium deposits at the base of the placenta, | Detection of chromosomal abnormalities, neural tube defects, and estimation of fetal lung maturity (L-S Ratio) |
Bishop Scoring
Labor may be induced, most often for post term babies via the use of oxytocic drugs. Augmentation of labor enhances labor in the cases of hypotonic contractions; prolonged labor. To determine the readiness of the pregnant client for induction or augmentation, Bishop Scoring is used.
The lowest score is 0, and the highest score is 13 (3, 3, 3, 2, 2). A score of 8 or above permits for induction/augmentation. Any lower and the doctor is not allowed to induce/augment labor. They may, however, proceed to promoting conditions to increase the Bishop score, e.g. promote cervical softening with prostaglandin gel, promote cervical dilatation with a laminaria tent, etc.
| Criteria | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Cervical Dilatation | 0 cm | 1–2 cm | 3–4 cm | 5–6 cm |
| Cervical Effacement | 0% to 30% | 40% to 50% | 60% to 70% | 80% or greater |
| Fetal Station | -3 | -2 | -1 to 0 | +1 to +2 |
| Cervical Consistency | Firm | Medium | Soft | N/A |
| Cervical Position | Posterior | Middle | Anterior | N/A |
- Determining Consistency: Firm (like tip of nose), Medium (like earlobe), Soft (like lips)
- The medicine used to “ripen” the cervix (induce Goodell’s sign) is a prostaglandin gel.
- If ineffective, Cytotec is used: a scored tablet with 100 mcg, usually administered as 1/4th of a tablet (25 mcg)
- If dilatation remains slow, a Laminaria Tent may be used. It is a dried, sterile, cone-shaped seaweed inserted into the cervix, where it absorbs cervical mucus and expands, facilitating dilatation.
- Determining Position: Posteriorly Positioned (cervix pointing to anus), Middle (straight), Anteriorly Positioned (cervix pointing to clitoris)
Cervical Consistency
Cervical consistency is the most important parameter of Bishop scoring, as its improvement will naturally also improve the other parameters, e.g., a softer cervix will efface and dilate better, and will allow fetal station to increase.
Fetal Distress
I made this section just to focus on fetal distress further. This was not explicitly part of the discussion.
Fetal distress occurs when a fetus fails to receive adequate oxygen in any condition. It may be caused by many factors, including (in no particular order):
- Uteroplacental insufficiency
- Abruptio placenta (placental separation)
- Placenta previa
- Fetal ketosis in Gestational Diabetes Mellitus
- Cord compression
- Tetanic contractions during labor (>90s)
- Preeclampsia
- Anemia
- Oligohydramnios (can also lead to cord compression)
- Placental degeneration in post-term clients
- Uterine rupture
- Abnormal fetal presentation
- Maternal stress
Assessment Findings
The following findings may be indicative or confirmatory of fetal distress (also in no particular order).
- Fetal Heart Rate: less than 100 BPM, normally 120 to 160 BPM.
- Decelerations: late or variable deceleration, normally early.
- Negative Nonstress Test is a warning sign. A Positive Nipple Stimulation Contraction Test is an ominous sign.
- Kick Count: less than normal in a 10 minute period. Normal activity is 5 to 15 kicks, average of 10 in 1 hour.
- Meconium-stained Amniotic Fluid is an automatic indication of fetal distress for non-breech fetuses. In breech-presented fetuses, alternative methods of determining distress is required as passing meconium during labor is expected from compression of the anal sphincter.
- Hyperactivity followed by hypoactivity in later distress.
- Tachycardia followed by bradycardia in later distress.
- Vaginal Bleeding is always an ominous sign in pregnancy, except for the expected show as a sign of true labor.
- Cramping or other abnormal contractions may place the fetus in distress.
Management
- Positioning: the mother is placed on a left-lateral position
- Oxygen therapy via face mask @ 5 to 8 L/min flow rate.
- Stop IV oxytocin (Syntocinon, Pitocin)
- Notify the physician.
- Place the patient on NPO status— they are a possible cesarean section.
Preoperative Preparation
(From previous discussion)
- Informed Consent Form
- NPO starting now
- Shaving the abdomen
- Removal: nail polish, dentures, jewelries, contact lenses (if possible)
- Endorse jewelries to the head, which they will endorse to the family member. Follow hospital protocol.
- Follow-up Lab Results, esp. CBC for blood preparations, blood typing, cross-matching.
- General Anesthesia may be used. Newborn APGAR score may be low and unconscious.
- If narcotic analgesics are used, Narcan should be prepared.
(From the perioperative lecture) Generally, these are the preoperative preparations to perform the day and night before the surgery:
- Pre-operative visit the day before the surgery.
- Client education on post-operative activities, such as breathing exercises to avoid pulmonary atelectasis, splinting coughs, etc.
- Complete laboratory and diagnostic examination coordinated with the MD.
- Cardiopulmonary (CP) Clearance: an initial evaluation to determine if the patient will be able to undergo surgical intervention on general anesthesia. Not being cleared indicates an elevated risk for cardiac events during surgery.
- Checking of blood products when indicated.
- Monitoring VS and I&O.
- Secure consent.
- Bathing as necessary.
- Light evening meal and NPO from midnight to the time of the surgery. No oral intake should be had to prevent emesis and pulmonary aspiration of gastric contents when placed under general anesthesia. Failure to maintain NPO status can be grounds for delaying surgery.
- Psychological and spiritual support.
- Administration of laxatives if indicated.
- Removal of nail polish (for accurate pulse oximetry).
On the morning of the surgery itself, the most important nursing actions include:
- Ensuring NPO for reasons previously mentioned.
- Oral care.
- Enema if ordered.
- Shaving areas to be operated on.
- Reviewing post-op exercises like those previously mentioned.
- Preoperative medications are also given at this time. They are discussed later in this section.
- Monitoring of patient status, including their psychological state. Provide support as necessary.
- Removal of dentures as aspiration precautions, jewelry, wigs, prosthetics(of possible), etc.
- Endorsement to the OR from the surgical ward.
Pre-operative medications are given to prepare the client for anesthesia and potentiate its effects, and to sedate the client to reduce anxiety levels. The anesthesiologist prepares the cocktail and the medication is given to the patient at least 30 to 60 minutes before the surgery. These include:
- Narcotic Analgesia: nubain (least potent), demerol, morphine (most potent)
- Sedatives: often phenergen
- Anticholinergics: to reduce the production of secretions. A common example is atrophine sulfate.